Case Study: Building a Stronger Emergency Response System in Limpopo

Strengthening Limpopo’s post-crash emergency response has been one of the most powerful achievements of the Limpopo Road Safety Programme (LRSP). Through a combined focus on updated clinical training, advanced rescue skills and improved operational systems, Projects 12 and 12.1 have reshaped how Emergency Medical Services (EMS) teams respond in the critical minutes after a crash – from the first emergency call to hospital handover.
Updating clinical skills to strengthen frontline emergency care
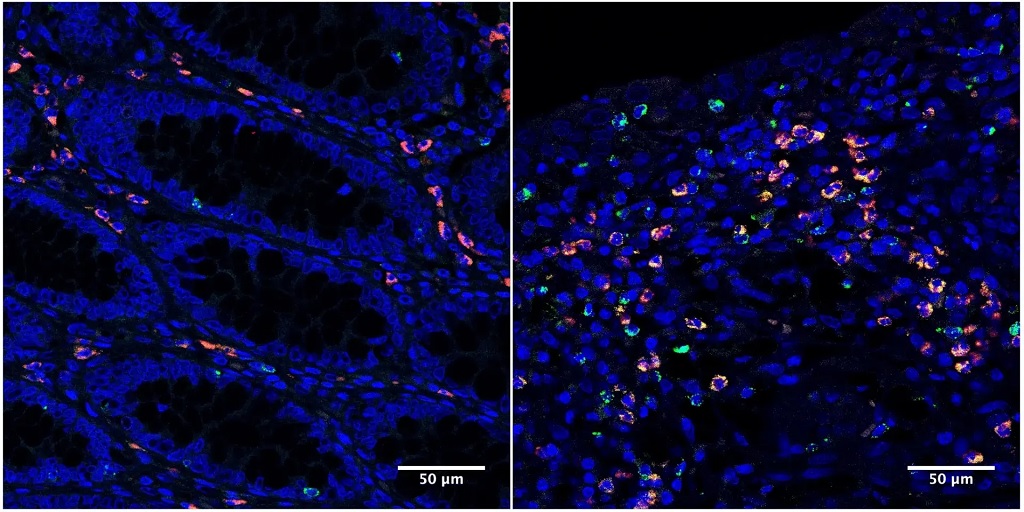
Across South Africa, the Clinical Practice Guidelines (CPGs) for emergency care have been substantially updated, including a major revision in 2018. These updates incorporated new evidence, improved patient outcomes, and standardised practice across the health system, shifting toward more user-friendly formats such as clinical decision-support tools. For Limpopo’s EMS, this presented both an opportunity and a challenge: although the guidelines were available, many personnel had not yet received training to apply them consistently in the realities of roadside emergencies. Project 12 addressed this need directly, rolling out comprehensive CPG training across all five districts. EMS practitioners were equipped with updated algorithms for trauma, medical, paediatric and obstetric emergencies, along with enhanced assessment, triage and stabilisation skills.
This clinical uplift aligned perfectly with major system improvements. In the 2023/2024 financial year, the Limpopo Department of Health procured more than 500 new, modern ambulances, significantly expanding the provincial fleet. The LRSP ensured this investment translated into real-world impact: EMS personnel were trained not only on updated CPGs but also to use the new vehicles and onboard equipment to their full potential; optimising monitoring, patient loading, scene workflow and en-route care. Modern ambulances combined with modern knowledge dramatically strengthened the quality of emergency care.
By 2025, the system advanced even further with the introduction of a Computer-Aided Dispatch (CAD) system, enabling more efficient call-taking, improved dispatch decision-making, clearer communication and better tracking of EMS resources across districts. The CAD system, together with updated CPGs and a modern ambulance fleet, created a tightly integrated platform for faster, smarter and more coordinated EMS response. For the first time, Limpopo could align clinical best practice, operational intelligence and fleet capacity into one cohesive system.
Introducing advanced rescue skills for high-severity crash scenes
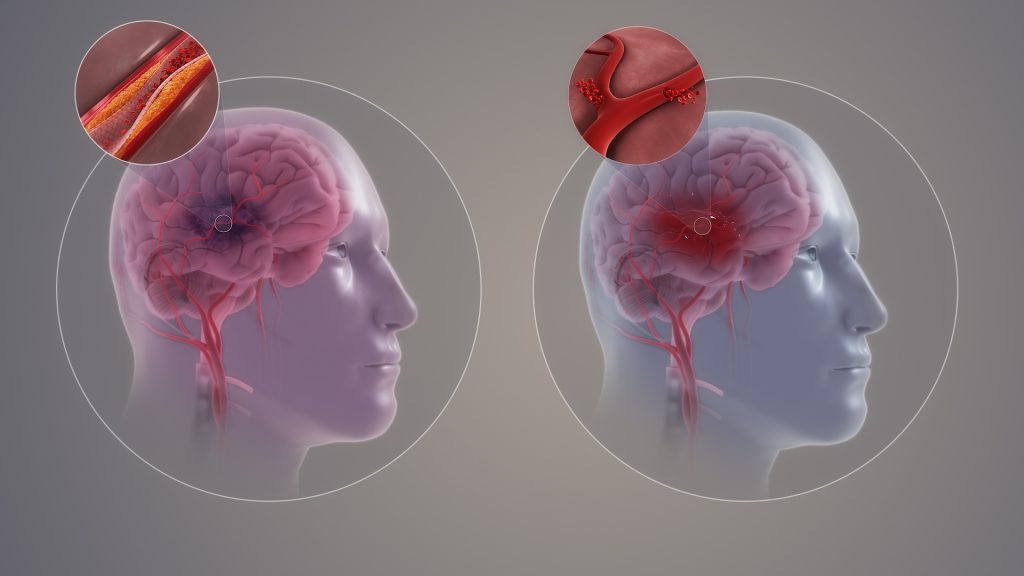
Yet, while clinical updates and dispatch improvements strengthened core EMS response, Limpopo still faced a critical need for specialised capacity at high-severity crash scenes, especially those involving vehicle entrapment. Project 12.1 filled this gap by introducing the province’s first Advanced Vehicle Rescue Short Course, delivered by EPIC EM and the University of Johannesburg. Over seven intensive days, participants trained in vehicle stabilisation, extrication techniques, hydraulic tool use, and multi-casualty scene management, blending theory with realistic, high-pressure simulations. Many described the training as transformative, giving them the competence and confidence to manage complex incidents on Limpopo’s regional and mining routes.
Together, these interventions have created a step change in Limpopo’s post-crash care system. Today, EMS teams arrive at crash scenes equipped with modern ambulances, updated clinical guidance, advanced rescue skills and a CAD-supported operational network that ensures faster and more coordinated response. Patients benefit from safer extrication, quicker stabilisation and better continuity of care during the “golden hour”. Beyond improving skills, the programme has strengthened morale, professionalism and a culture of excellence within EMS.
Projects 12 and 12.1 have left a lasting legacy: a provincial emergency response system that is smarter, faster and better prepared to save lives on Limpopo’s roads.