Certain Gut Bacteria Assist in Immunotherapy for Milk Allergy
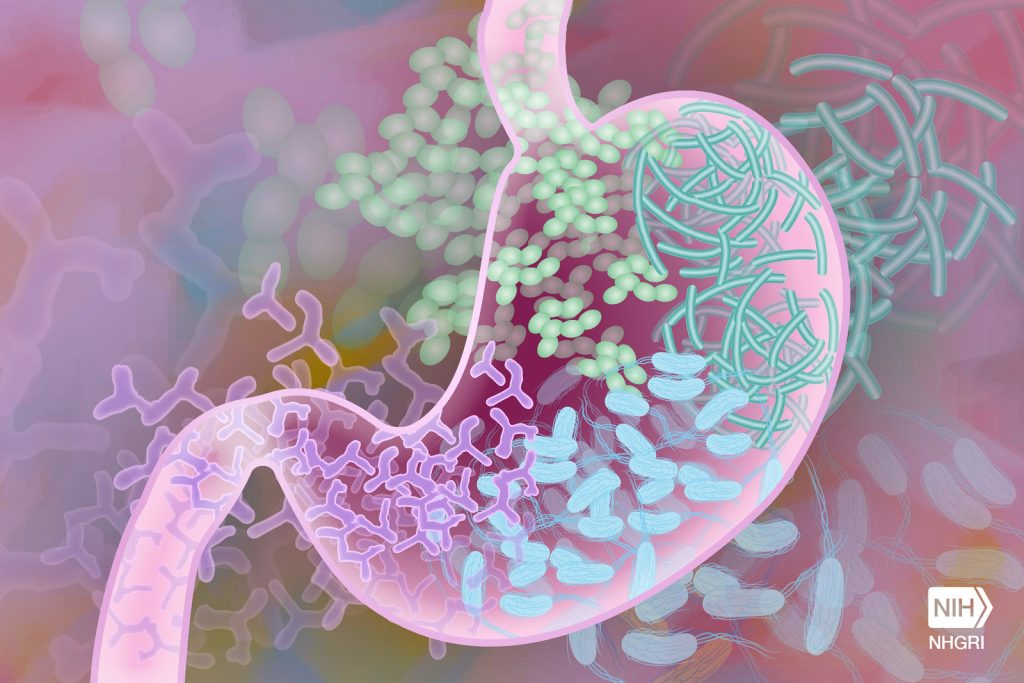
Researchers in Japan have discovered a link between gut bacteria and the success of milk-allergy oral immunotherapy. Published in the scientific journal Allergology International, the study found that Bifidobacterium – a genus of beneficial bacteria in the gut – was associated with a higher chance of successful treatment. The finding may help in the development of more effective oral immunotherapies, perhaps by combining them with probiotic supplements.
Many children have allergic reactions to certain milk proteins. Most grow out of it but some have to contend with lifelong allergy. Milk allergy can be improved by oral immunotherapy – taking small, increasing doses of milk. Unfortunately, while allergic reactions are controlled during treatment, in most cases, tolerance disappears soon after the treatment ends.
Gut bacteria are thought to help reduce allergic reactions to some foods, but little is known about the link between these bacteria and oral immunotherapy for milk allergy. Hiroshi Ohno led a team at the RIKEN Center for Integrative Medical Sciences to find out why. The researchers examined 32 children with cow’s milk allergy who received oral immunotherapy, with the first month being conducted in a hospital. “Oral immunotherapy is not without risk,” explains Ohno. “We closely monitored the children in the hospital, and in fact 4 children had such severe reactions to the milk that we could not allow them to continue the treatment.”
The remaining 28 children then completed an additional 12 months of treatment at home. Next, they avoided milk for two weeks, and were then tested on a double-blind, placebo-controlled food challenge to see if they could still tolerate milk without any allergic reactions. During the food challenge, children were initially given a tiny amount of placebo or milk (only 0.01mL) which was gradually increased every 20 minutes until they had an allergic reaction or until they could drink the final 30mL without a reaction.
The researchers focused their analyses on immunological and bacterial changes during the treatment and the relationship between gut bacteria and successful treatment—which was defined as showing milk tolerance that lasted beyond the treatment period by passing the food challenge. They found that during treatment, immunological markers for cow’s milk allergy improved, and bacteria in the gut changed. Nevertheless, after two weeks of avoiding milk, only 7 of the 28 children passed the food challenge, even though they had been able to drink milk safely at the end of the treatment.
To understand why the treatment worked for these seven children but not the others, the team looked for the clinical factors and types of gut bacteria that were related to successful treatment. Of the clinical factors, unsuccessful treatment was more likely in children who were being treated for eczema or asthma and in children who initially had higher levels of milk-protein antibodies. Among the gut bacteria, the presence of Bifidobacterium, a genus of beneficial bacteria in the Bifidobacteriaceae family was related to a higher chance of successful treatment. In fact, only children who passed the final food challenge showed an increasing trend in these bacteria over the course of treatment. When considering ways to improve oral immunotherapy, this is good news because while the first two factors are difficult to change, the types of bacteria in one’s gut are not set in stone.
“With this study, we have identified gut environmental factors that help establish immune tolerance against cow’s milk allergy via oral immunotherapy,” says Ohno. “The next step is to examine the mechanisms underlying this phenomenon and to develop ways to improve the effectiveness of oral immunotherapy, such as the addition of probiotic supplements.”
Source: RIKEN







