Old Blood Pressure Drug, New Tumour-fighting Tricks
A Penn-led team has revealed a how hydralazine, one of the world’s oldest blood pressure drugs and a mainstay treatment for preeclampsia, works at the molecular level. In doing so, they made a surprising discovery – it can also halt the growth of aggressive brain tumours.
Over the last 70 years, hydralazine has been an indispensable tool against life-threatening high blood pressure, especially during pregnancy. But despite its essential role, a fundamental mystery has persisted: No one knows its mechanism of action, which allows for improved efficacy, safety, and what it can treat.
“Hydralazine is one of the earliest vasodilators ever developed, and it’s still a first-line treatment for preeclampsia – a hypertensive disorder that accounts for 5-15% of maternal deaths worldwide,” says Kyosuke Shishikura, a physician-scientist at the University of Pennsylvania. “It came from a ‘pre-target’ era of drug discovery, when researchers relied on what they saw in patients first and only later tried to explain the biology behind it.”
Now Shishikura, his postdoctoral adviser at Penn Megan Matthews, and collaborators have solved this long-standing puzzle.
In a paper published in Science Advances, the team uncovered the method of action of hydralazine, and in doing so, revealed an unexpected biological link between hypertensive disorders and brain cancer. The findings highlight how long-established treatments can reveal new therapeutic potential and could help in the design of safer, more effective drugs for both maternal health and brain cancer.
“Preeclampsia has affected generations of women in my own family and continues to disproportionately impact Black mothers in the United States,” Matthews says. “Understanding how hydralazine works at the molecular level offers a path toward safer, more selective treatments for pregnancy-related hypertension—potentially improving outcomes for patients who are at greatest risk.”
Hydralazine blocks an oxygen-sensing enzyme
The team found that hydralazine blocks an oxygen-sensing enzyme called 2-aminoethanethiol dioxygenase (ADO) – a molecular switch for blood vessels contraction.
“ADO is like an alarm bell that rings the moment oxygen starts to fall,” Matthews says. “Most systems in the body take time; they have to copy DNA, make RNA, and build new proteins. ADO skips all that. It flips a biochemical switch in seconds.”
Hydralazine acts by binding to and blocking ADO – effectively “muting” that oxygen alarm. Once the enzyme was silenced, the signaling proteins it normally degrades – called regulators of G-protein signaling (RGS) – remained stable.
The buildup of RGS proteins, says Shishikura, tells the blood vessels to stop constricting, effectively overriding the “squeeze” signal. This reduces intracellular calcium levels, which he calls the “master regulator of vascular tension.” As calcium levels fall, the smooth muscles in blood vessel walls relax, causing vasodilation and a drop in blood pressure.
From preeclampsia to brain cancer: A common target
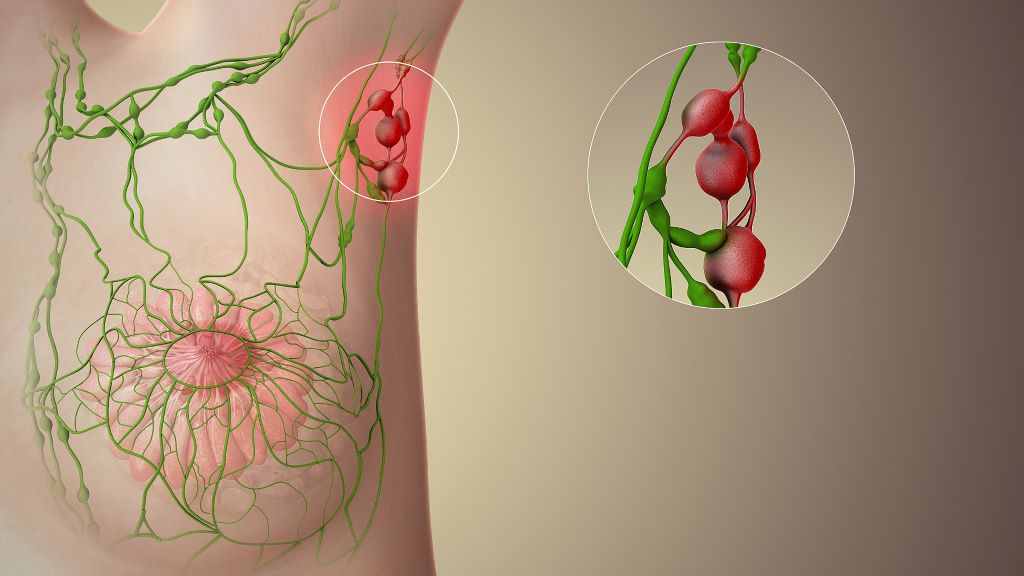
Prior to this study, cancer researchers and clinicians had begun to suspect that ADO was important in glioblastoma, where tumours often have to survive in pockets of very low oxygen, Shishikura explains. Elevated levels of ADO and its metabolic products had been linked with more aggressive disease, suggesting that shutting this enzyme down could be a powerful strategy, but no one had a good inhibitor to test that idea.
To see if hydralazine was a contender, Shishikura worked closely with structural biochemists at the University of Texas, who used X-ray crystallography to visualise hydralazine bound to ADO’s metal centre, and with neuroscientists at the University of Florida, who tested the drug’s effects in brain cancer cells.
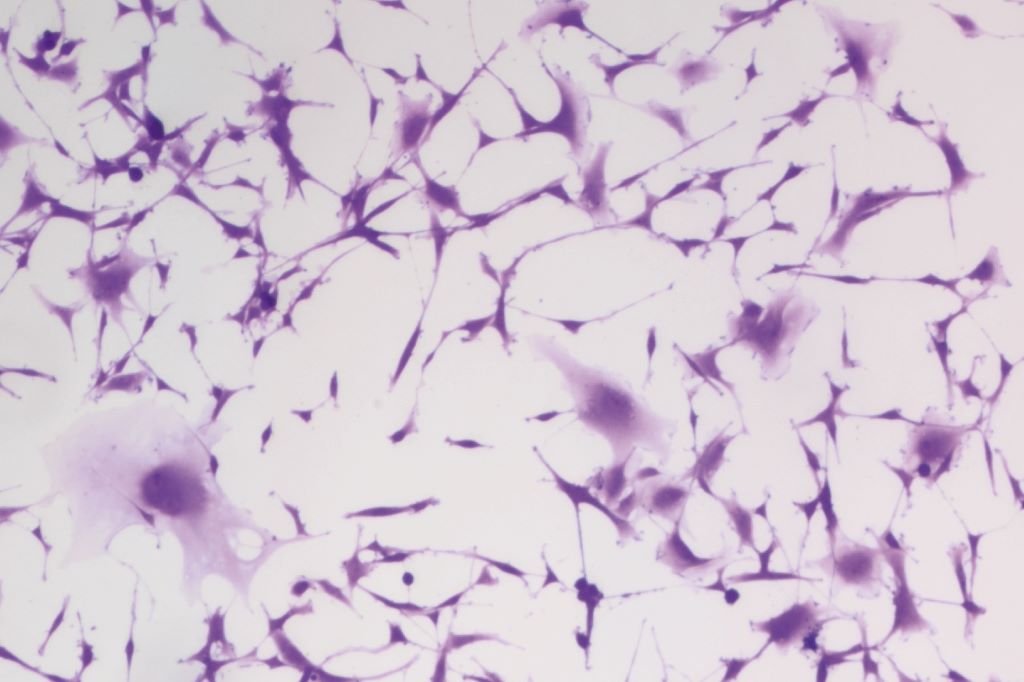
They found that the ADO pathway that regulates vascular contraction also helps tumour cells survive in low-oxygen environments. Unlike chemotherapy, which aims to kill all cells outright, hydralazine disrupted that oxygen-sensing loop, triggering cellular senescence.
Unlocking the potential for other lifesaving treatments
Their findings highlight how long-established treatments can reveal new therapeutic potential and could help in the design of safer, more effective drugs for both maternal health and brain cancer.
They say the next step is to push the chemistry further building new ADO inhibitors that are more tissue specific and better at crossing, or exploiting weak points in, the blood-brain barrier so they hit tumour tissue hard while sparing the rest of the body.
Matthews is also working to continue engineering the next generation of medical solutions by revealing the mechanics of clinically tested, long-known treatments.
“It’s rare that an old cardiovascular drug ends up teaching us something new about the brain,” Matthews says, “but that’s exactly what we’re hoping to find more of – unusual links that could spell new solutions.”
Source: University of Pennsylvania