Brain Study Prompts a Rethink of Alcohol Abuse and Relapse

What compels someone to keep engaging in alcohol use, even if it damages their health, relationships and wellbeing? A new study from Scripps Research offers an important clue: a small midline brain region plays a key role in how animals learn to continue drinking to avoid the stress and misery of withdrawal.
In a new study, published in Biological Psychiatry: Global Open Science on August 5, 2025, the Scripps Research team zeroed in on a set of brain cells in the paraventricular nucleus of the thalamus (PVT) in rats. They found that this region becomes more active, driving strong relapse behaviour, when rats learn to associate environmental stimuli with the easing of withdrawal symptoms by alcohol. By illuminating this brain pathway, the research sheds light on one of the most stubborn features of addiction – drinking not for pleasure, but to escape pain – and could eventually lead to new treatments for substance use disorders (SUDs) as well as other maladaptive behaviours including anxiety.
“What makes addiction so hard to break is that people aren’t simply chasing a high,” says Friedbert Weiss, professor of neuroscience at Scripps Research and senior author of the study. “They’re also trying to get rid of powerful negative states, like the stress and anxiety of withdrawal. This work shows us which brain systems are responsible for locking in that kind of learning, and why it can make relapse so persistent.”
“This brain region just lit up in every rat that had gone through withdrawal-related learning,” says co-senior author Hermina Nedelescu of Scripps Research. “It shows us which circuits are recruited when the brain links alcohol with relief from stress – and that could be a game-changer in how we think about relapse.”
From behaviour to brain maps
An estimated 14.5 million people in the United States have alcohol use disorder, which encompasses a range of unhealthy drinking behaviours. Like other drug addictions, alcohol addiction is characterised by cycles of withdrawal, abstinence and relapse.
In 2022, Weiss and Nedelescu used rats to study the types of learning that happen in the brain throughout this cycle. When rats initially begin drinking, they learn to associate pleasure with alcohol and seek more. However, that conditioning becomes far stronger during multiple cycles of withdrawal and relapse. After learning that alcohol eased the unpleasant feelings of withdrawal – negative reinforcement, or a relief of ‘negative hedonic state’ – the animals sought out more alcohol and would remain persistent even when uncomfortable.
“When rats learn to associate environmental stimuli or contexts with the experience of relief, they end up with an incredibly powerful urge to seek alcohol in the presence of that stimuli –even if conditions are introduced that require great effort to engage in alcohol seeking,” says Weiss. “That is, these rats seek alcohol even if that behavior is punished.”
In the new work, the team wanted to pin down exactly what networks of cells in the brain were responsible for learning to associate environmental cues with the relief of this negative hedonic state.
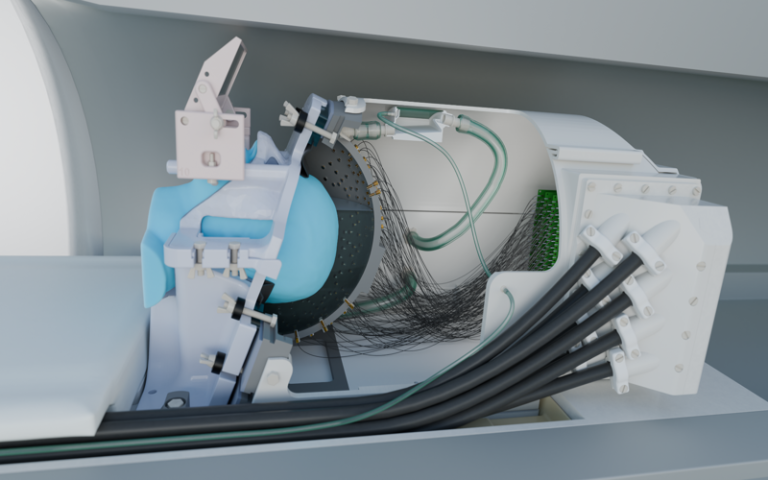
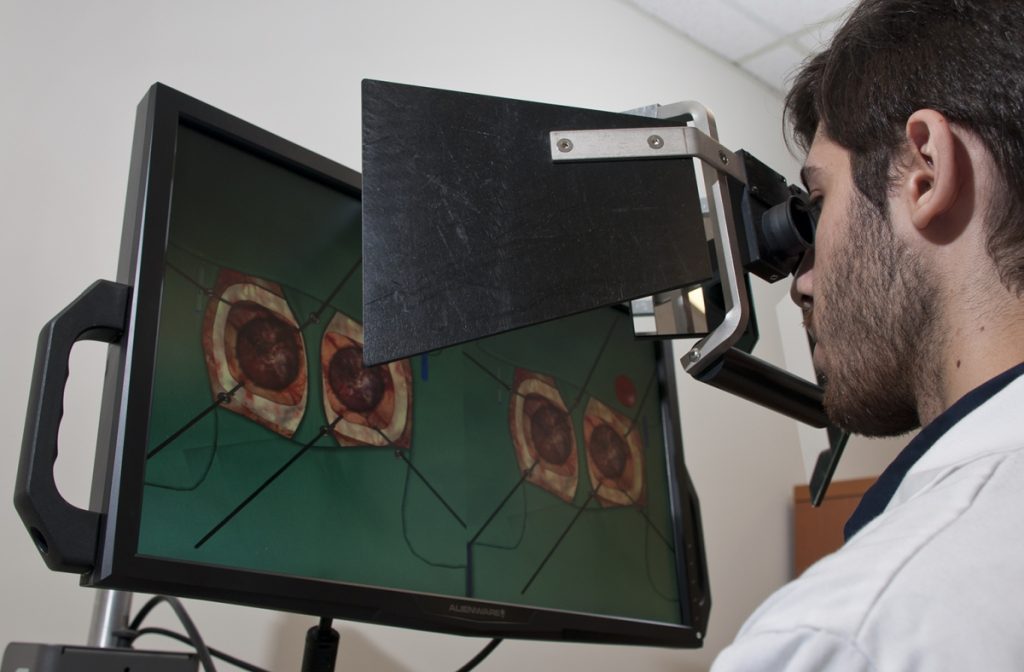
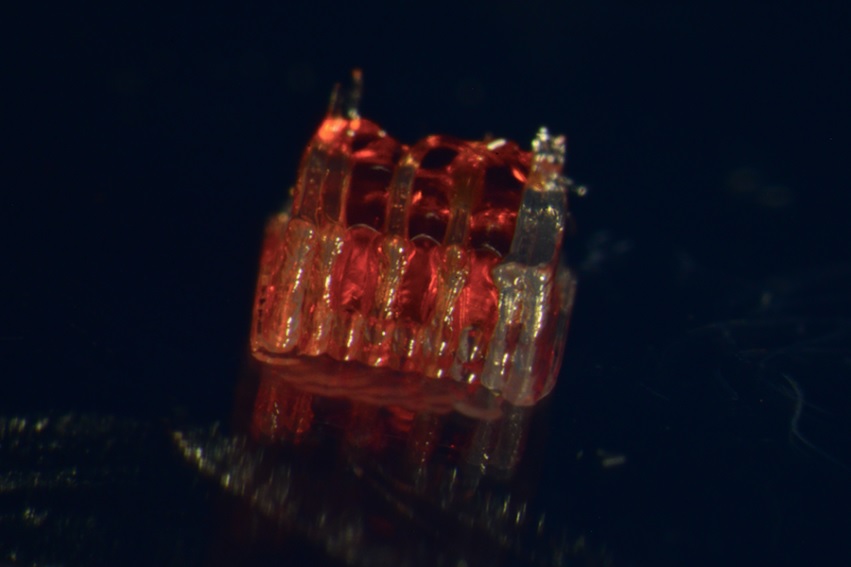
The researchers used advanced imaging tools to scan entire rat brains, cell by cell, and pinpoint areas that became more active in response to alcohol-related cues. They compared four groups of rats: those that had gone through withdrawal and learned that alcohol relieves a negative hedonic state, and three different control groups that had not.
While several brain areas showed increased activity in the withdrawal-learned rats, one stood out: the PVT, which is known for its role in stress and anxiety.
“In retrospect, this makes a lot of sense,” says Nedelescu. “The unpleasant effects of alcohol withdrawal are strongly associated with stress, and alcohol is providing relief from the agony of that stressful state.”
The researchers hypothesise that this negative hedonic state, and the activation of the PVT in the brain as a response, is critical for how the brain learns and perpetuates addiction.
A better understanding of addiction
The implications of the new study extend well beyond alcohol, the researchers say. Environmental stimuli conditioned to negative reinforcement – the drive to act in order to escape pain or stress – is a universal feature of the brain, and can drive human behaviour beyond substance use disorders such as anxiety disorders, fear-conditioning and traumatic avoidance learning.
“This work has potential applications not only for alcohol addiction, but also other disorders where people get trapped in harmful cycles,” says Nedelescu.
Future research will zoom in even further. Nedelescu and colleagues at Scripps Research want to expand the study to females and to study neurochemicals released in the PVT when subjects encounter environments associated with the experience of this relief from a negative hedonic state. If they can pinpoint molecules that are involved, it could open new avenues for drug development by targeting those molecules.
For now, the new study underscores a key shift in how basic scientists think about addiction.
“As psychologists, we’ve long known that addiction isn’t just about chasing pleasure – it’s about escaping those negative hedonic states,” says Weiss. “This study shows us where in the brain that learning takes root, which is a step forward.”
Source: Scripps Research