‘Sweet Spot’ for Focused Ultrasound Provides Relief from Essential Tremor

Essential tremor, a common neurological movement disorder, causes uncontrollable shaking, most often in the hands, but it can also occur in the arms, legs, head, voice, or torso. Essential tremor impacts an estimated 1% of the worldwide population and around 5% of people over 60.
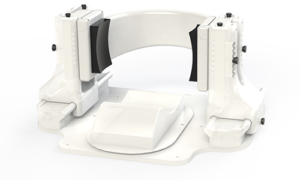
Investigators from Mass General Brigham identified a specific subregion of the brain’s thalamus that, when included during magnetic resonance-guided focused ultrasound (MRgFUS) treatment, can result in optimal and significant tremor improvements while reducing side effects. Their results are published in Science Advances.
“This one-time, noninvasive treatment can have immediate, long-lasting and lifechanging effects for patients and was pioneered here at Brigham and Women’s Hospital 30 years ago,” said co-senior author G. Rees Cosgrove, MD, FRCSC, director of functional neurosurgery at Brigham and Women’s Hospital. “The results of this study will help make the procedure even more safe and effective than it already is and will help other centres around the world improve their outcomes.”
MRgFUS treatment of essential tremor creates a small, permanent lesion in a specific nucleus in the thalamus that is thought to be part of the brain circuit mediating the disorder and disrupts the tremor-causing activity. The research team analysed data from 351 thalamotomy patients that were treated across three international hospitals, the largest cohort assessed to date, to identify the optimal location for this procedure and better understand its impacts on clinical improvements and side effects.
The study identified a set of optimal sites and brain connections to target, as well as locations and connections to avoid that lead to side effects. The team then tested whether this ‘sweet spot’ could be used as a model to predict the outcomes in a cohort of patients treated with the same procedure at another centre, which proved true. The more the ‘sweet spot’ was lesioned, the better the outcome was in all patients’ one-year, post-procedure comparison data. According to the researchers, when thalamotomy patients have good tremor control at one year, it is typically sustained over multiple years.
“Seeing how this procedure can make such a huge impact on patients’ lives is what motivated me to pursue this research,” said lead author Melissa Chua, MD, a senior resident in the Brigham’s Department of Neurosurgery. “It is very exciting to have such robust validation and to be moving toward this treatment becoming even more precise and personalized in the future.”
Next, the team plans to further analyse patient data for a more detailed picture of the evolution of this technology and how patient outcomes have improved, to fully understand the parameters that go into achieving long-term tremor control and minimise side effects.
“It is incredible when you can provide a patient with relief from these tremors,” Cosgrove said. “It is like a gift when patients who have not been able to sing, speak in public, write, or even drink from a cup for years can once again do so – we see it in case after case.”
Source: Mass General Brigham