Vigorous Exercise Improves Walking in Chronic Stroke Patients

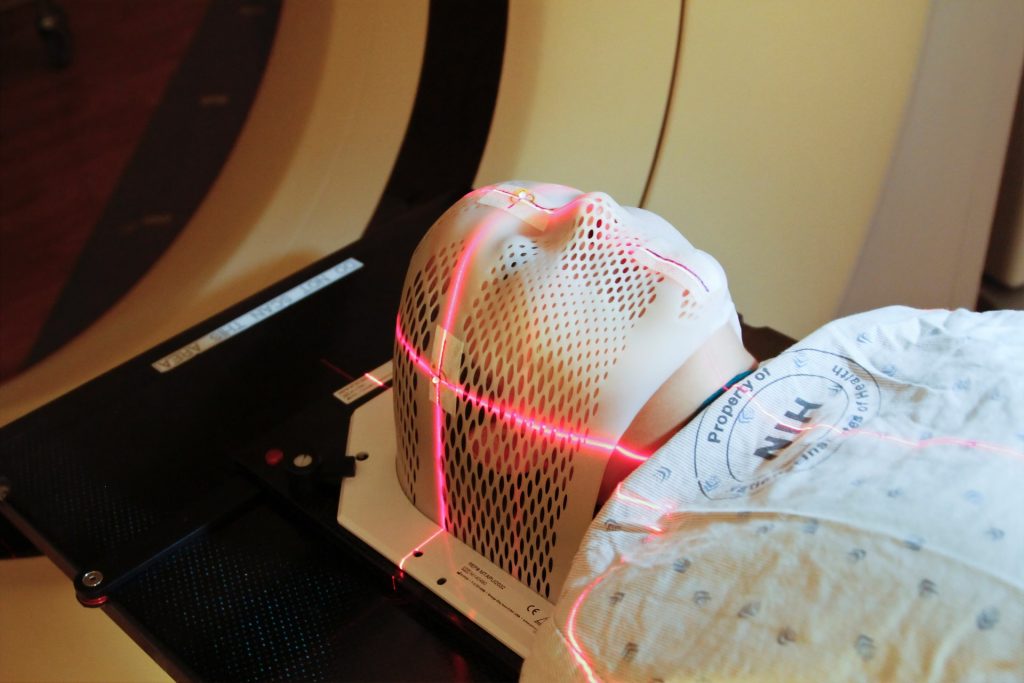
When 67-year-old Larry Christian suffered a sudden loss of balance, he was diagnosed with a haemorrhagic stroke, and referred to the University of Delaware’s Physical Therapy Clinic for rehabilitation.
“Initially, I had a lot of balance problems that we worked pretty intensely to correct,” Christian said.
He enrolled in a clinical trial at UD, led by co-investigator Darcy Reisman, professor and chair of the Department of Physical Therapy, that sought to explore whether high-intensity interval training (HIIT) aids in improved gait post-stroke. UD was one of three sites selected for the clinical trial led by primary investigator and associate professor Pierce Boyne of the University of Cincinnati. Sandra Billinger, professor and vice chair of stroke translation research at the University of Kansas Medical Center, is also a co-investigator and represents the third site involved in the clinical trial.
Now, seven years later, Christian is walking better.
“Participating in this study got me to a point where I could walk better and even take a walk outside,” Christian said. “I’ve been pretty healthy all my life, and while I can’t play volleyball anymore, walking again made me feel great.”
Christian is among the lucky ones. Among 7 million stroke survivors in the US, fewer than 10% have adequate walking speed and endurance to complete normal daily activities like grocery shopping.
Reisman said the results of the multi-million-dollar, five-year clinical trial showed HIIT helped more people than just Christian. The results, published in JAMA Neurology, show that chronic stroke survivors who engaged in high-intensity exercise with bursts of maximum-speed walking alternated with recovery periods saw a significant difference in their walking capacity over 12 weeks. The improvements were so dramatic Boyne and Reisman have secured a clinical trial grant renewal to triple the size of their study to 165 participants.
She added HIIT looks different for each stroke survivor, and the optimal exercise program for each person with stroke remains unknown.
“We want them to train at the fastest possible speed, which varies from person to person,” Reisman said. “But we don’t want them running.”
For those already walking at a reasonably fast pace, research associate Henry Wright in Reisman’s lab will add an incline or a weighted vest or wrap a bungee cord around their waist to create resistance.
“It’s self-reported data, but participants tell me they have more energy, or they’re able to do more around the house, or they’re not winded when they go shopping,” Wright said. “By the end of the training, I can see their walking is smoother, they’re getting farther on clinical testing, and it’s rewarding to see their gains.”
The results from the initial clinical trial showed Reisman and collaborators that HIIT was feasible and safe in a small group of stroke survivors, who saw sustained gains in walking capacity, more so than patients engaged in moderate-intensity exercise.
However, further study of the intervention in larger populations is crucial to change the standard of care.
“Many physical therapists were trained during a time when patients with neurologic conditions, particularly stroke, were treated with kid gloves, partly because they say stroke is the heart attack of the brain,” Reisman said. “It’s common they also have cardiovascular conditions, so people tend to be extra careful with those patients in terms of pushing them.
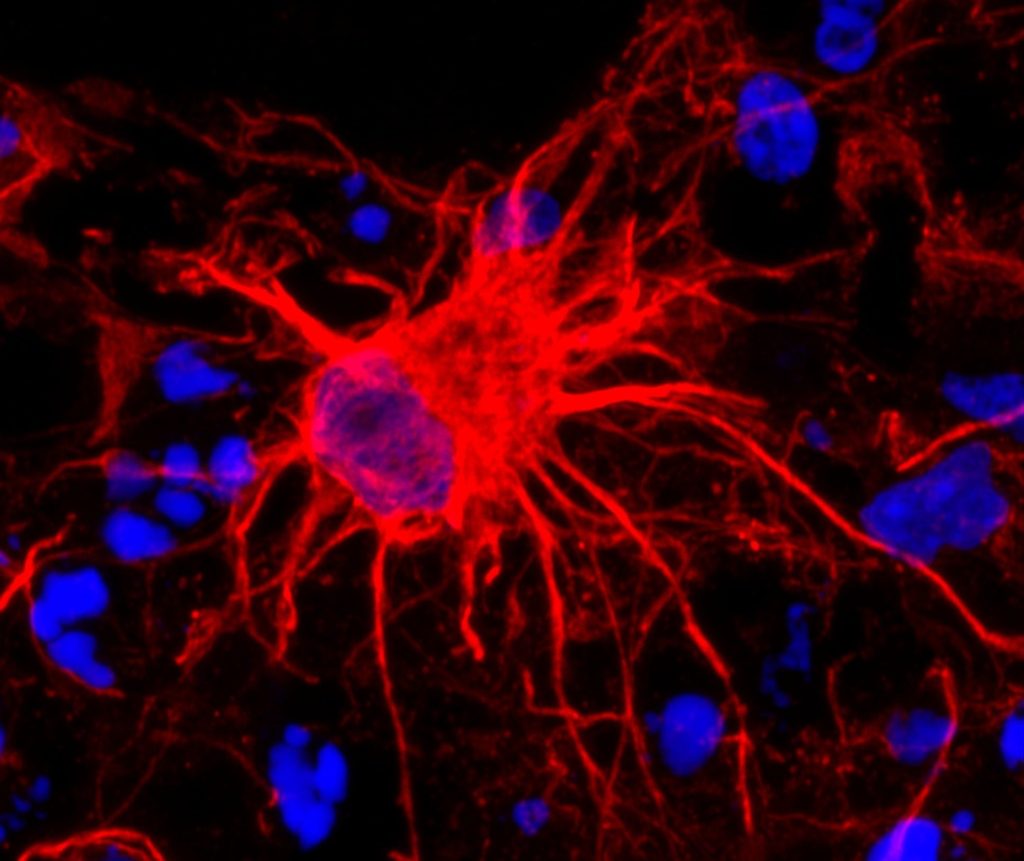
“But what we know now is at least moderate-intensity, and likely high-intensity interval training, is essential not only for stroke survivors’ cardiovascular system but also for their brain,” Reisman said. “The evidence shows that intensity is linked to the release of neurotrophins in the brain that help the brain remodel after a stroke.”
Kiersten McCartney, a physical therapist obtaining her doctorate in biomechanics and movement science, worked on the clinical trial with Reisman. She spent the 2022 Winter Session at Magee Rehabilitation Hospital in Philadelphia, helping them implement moderate-to-high-intensity exercise and saw the benefits first-hand.
“I’ll never be able to say there’s no risk of heart attack. Even the fittest people can have a heart attack when exercising,” McCartney said. “Still, the data points to the idea that you’re doing more harm than good by not engaging your patients with stroke in high-intensity exercise when we talk about those longer-term outcomes.”
The HIIT-Stroke Trial 2 will continue to examine dosing to confirm whether a full 12 weeks of vigorous exercise is needed to see significant improvements in walking. Reisman and collaborators will identify whether differences in sex and other factors played a role in rehabilitation. If the five-year study results are similar and show significant gains from high-intensity interval exercise in a larger population, investigators would next work with NIH Strokenet to launch a nationwide clinical trial in people with stroke.
“We’ve known about the value of moderate-intensity exercise for more than a decade, and it’s still not the standard of care,” Reisman said. “If we find that HIIT is the optimal intervention, the next phase would be the knowledge translation phase, where we’d systematically develop a methodology to get HIIT into clinics.”
For HIIT to work as an intervention, Reisman said therapists will need the proper tools. She’s been pushing for commercially available heart rate monitors, placed around the chest during exercise, to be the standard of care in clinics for years.
“They’re already a standard of care for people in the community,” Reisman said. “Getting them into clinics is imperative so PTs can monitor patients’ heart rate the entire time they exercise. That constant monitoring gives therapists data on how a person is responding beyond visible signs and symptoms, and in turn, more peace of mind.”
But beyond tools and training, Reisman said, it comes down to evidence and education.
“If we have hundreds and hundreds of stroke survivors who’ve gone through our high-intensity exercise intervention, and we’ve seen no major adverse events – that will help,” Reisman said. “The more data we have to show therapists, the better we can implement this intervention that will change lives.”
Source: University of Delaware