Less Invasive Method for Measuring Intracranial Pressure After TBI

Researchers at Johns Hopkins explored a potential alternative and less-invasive approach to evaluate intracranial pressure (ICP) in patients with serious neurological conditions. This research, using artificial intelligence (AI) to analyse routinely captured ICU data, was published in Computers in Biology and Medicine.
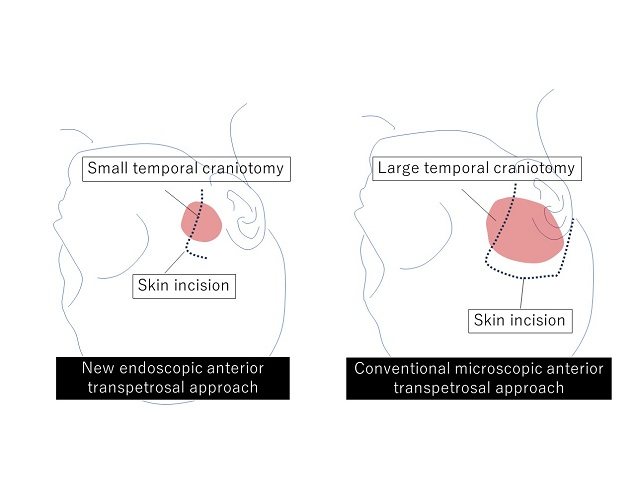
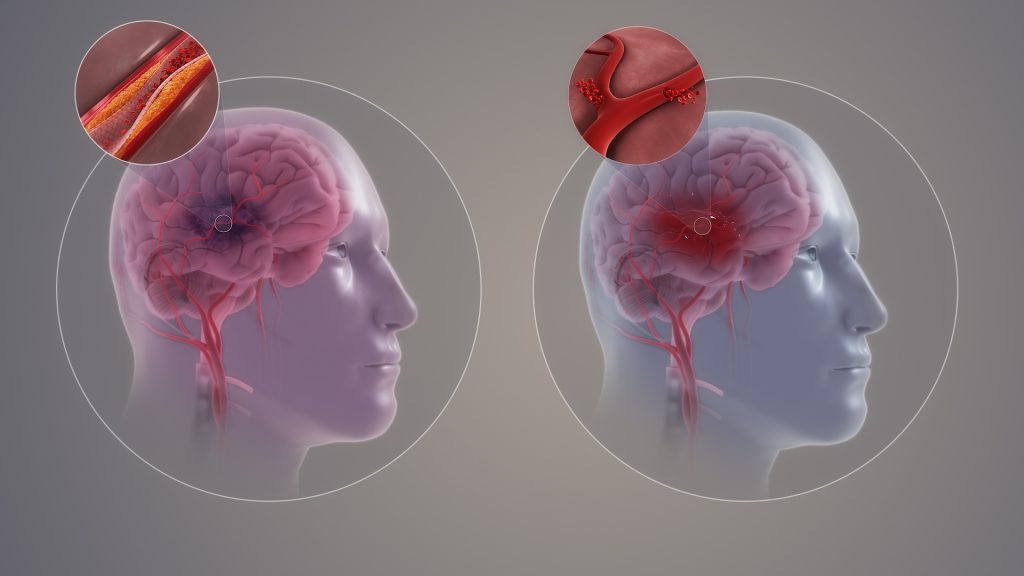
ICP is a physiological variable that can increase abnormally if one has severe traumatic brain injury, stroke or obstruction to the flow of cerebrospinal fluid. Symptoms of elevated ICP may include headaches, blurred vision, vomiting, changes in behaviour and decreased level of consciousness. It can be life-threatening, hence the need for ICP monitoring in selected patients who are at increased risk. But the current standard for ICP monitoring is highly invasive: it requires the placement of an external ventricular drain (EVD) or an intraparenchymal brain monitor (IPM) in the functional tissue in the brain consisting of neurons and glial cells by drilling through the skull.
“ICP is universally accepted as a critical vital sign – there is an imperative need to measure and treat ICP in patients with serious neurological disorders, yet the current standard for ICP measurement is invasive, risky, and resource-intensive. Here we explored a novel approach leveraging Artificial Intelligence which we believed could represent a viable noninvasive alternative ICP assessment method,” says senior author Robert Stevens, MD, MBA, associate professor of anaesthesiology and critical care medicine.
EVD procedures carry a number of risks including catheter misplacement, infection, and haemorrhaging at 15.3 %, 5.8 %, and 12.1 %, respectively, according to recent research. EVD and IPM procedures also require surgical expertise and specialised equipment that is not consistently available in many settings thus underscoring the need for an alternative method in examining and monitoring ICP in patients.
The Johns Hopkins team, a group that included faculty and students from the School of Medicine and Whiting School of Engineering, hypothesised that severe forms of brain injury, and elevations in ICP in particular, are associated with pathological changes in systemic cardiocirculatory function due, for example, to dysregulation of the central autonomic nervous system. This hypothesis suggests that extracranial physiological waveforms can be studied to better understand brain activity and ICP severity.
In this study, the Johns Hopkins team set out to explore the relationship between the ICP waveform and the three physiological waveforms that are routinely captured in the ICU: invasive arterial blood pressure (ABP), photoplethysmography (PPG) and electrocardiography (ECG). ABP, PPG and ECG data were used to train deep learning algorithms, resulting in a level of accuracy in determining ICP that rivals or exceeds other methodologies.
Overall study findings suggest a completely new, noninvasive alternative to monitor ICP in patients.
Stevens says, “with validation, physiology-based AI solutions, such as the one used here, could significantly expand the proportion of patients and health care settings in which ICP monitoring and management can be delivered.”
Source: John Hopkins Medicine