Janet Giddy | If COVID-19, Why not TB? Mr President, it’s Time for a Family Chat

By Janet Giddy
South Africa had several “family chats” in which President Cyril Ramaphosa addressed the nation during the height of the COVID-19 pandemic. He should do the same for tuberculosis, argues Dr Janet Giddy of the advocacy group TB Proof.
Recently, I was flying home and got chatting to the stylishly dressed woman in the window seat next to me. We asked each other the sort of questions that traveller’s often do. Suzie (name changed) was going to Cape Town to facilitate an artist’s workshop. I told her that I worked for an NGO that did tuberculosis (TB) research and advocacy. Suzie nodded pensively, then said: “My dad had TB”. I was just thinking how to respond, when she added: “he died from it”.
I have conversations about TB almost every day, and have previously written about high-altitude chats with fellow travellers. I get into these conversations not because TB work is my “day job” – which it is – but because I am a TB activist, and a survivor of childhood TB.
There are many remarkable things about TB that keep me engaged, enraged and activated. For example, that 29 934 people were diagnosed with TB in 2024 in the Cape Town metro, which was more than the combined number diagnosed with TB in the whole of the United States (10 347), the United Kingdom (5 480), France (4 217), and Canada (1 258). The population of these four countries combined is over 500 million, while Cape Town has a population of just under five million people. If you do the math, the risk of getting TB clearly depends massively on where you live. If these figures do not shock you, they should.
Why are so many people in South Africa unaware and seemingly unconcerned about the extraordinarily high numbers of people infected with TB in our country? Could we take TB more seriously as a country? My answer is yes.
If COVID-19, why not TB?
As expected, South Africa worked up a huge head of steam at every level of society about COVID-19. I think back on President Cyril Ramaphosa’s regular avuncular “family chats” to the nation. In the first COVID-19 “family chat”, our president told us:
“This is a decisive measure to save lives of South Africans from infection and save the lives of hundreds of thousands of our people. While this measure will have a considerable impact on people’s livelihoods, and on the life of our society and on our economy, the human cost of delaying this action would be far, far greater.”
Why has Ramaphosa not ever spoken in this intimate “family style” way to the nation about how important or urgent it is to tackle TB? A disease which continues to cause significantly more suffering and death than COVID-19 did.
In 2018, our president spoke to the international world about TB, when he addressed the President of the General Assembly of the United Nations (UN) and Director-General of the World Health Organization at the first ever UN High-Level Meeting on Tuberculosis. With great gravitas and in oratorial style, Ramaphosa said: “This … is a historic opportunity that we must embrace if we are to effectively respond to a disease that has killed more people than smallpox, malaria, the plague, influenza, HIV and AIDS, and Ebola combined. This meeting is taking place in the year of the centenary of the birth of South Africa’s founding President, Nelson Mandela. President Mandela was a survivor of tuberculosis, which he contracted while in prison, and was firmly committed to the campaign against the disease.”
Ramaphosa went on to highlight the social determinants of TB, including poverty, unemployment, poor nutrition, overcrowding and social stigma that fuel the spread of diseases. He also noted: “In South Africa, TB is the biggest cause of mortality in the general population, especially among men.”
This was an excellent message, but since 2018, our president has not had much to say about TB in public or to South Africans. It would be powerful and impactful if he were to talk about TB as a national emergency that requires a coordinated “family response” as a nation.
In considering the seriousness of TB as compared to COVID-19, let’s look at mortality.
By November 2022, the official number of deaths recorded as being due to COVID-19 in South Africa was around 102 000, approximately 34 000 per year when averaged out. Official numbers are however widely considered to be an underestimate. The Medical Research Council estimated in the region of 300 000 excess deaths relating to COVID-19 from 2020 to 2022, with around 85 000 in 2020, 200 000 in 2021, and around 15 000 a few months into 2022. Not all of these excess deaths would have been directly due to COVID-19, but it is likely that over 80% was (say 240 000 over the three years).
By comparison, TB has in recent years been claiming between 50 000 and 70 000 lives per year, based on estimates from the World Health Organization (WHO) and the Thembisa mathematical model. Thus, while there were many more COVID-19 deaths in 2021 than there were TB deaths, TB deaths almost certainly surpassed COVID-19 deaths in 2022 and subsequent years. The more one zooms out, the more the steady torrent of TB deaths over the last five, 10, 20 years, dwarfs the spike in COVID-19 deaths around 2021.
‘We are all at risk’
Back to my recent high-altitude chat in the plane: somehow, it was a uniquely South African sort of conversation. What is the chance that, while cruising at 10 000 meters over the Atlantic on a flight between the United States and France, that you’d sit next to someone whose parent recently died of TB? An extremely small chance. So, I would contend that all South Africans do need to know about TB, which is a disease that affects families profoundly.
It’s time for South Africa to have family chats about TB. There are many reasons to have these chats, starting with the fact that we are all at risk of getting it, given that we live in a country with a high TB prevalence – it was estimated that 389 people per 100 000 in South Africa fell ill with TB in 2024. We could compare this with the 2024 figures for the United Kingdom, at 9.7 per 100 000, which is higher than the United States’ rate of 3.2 per 100 000. For those who are interested, you can look up the latest numbers for different countries on the WHO’s excellent TB data portal.
The bottom line is that the higher the TB prevalence in the country you live in, the more chance that you or a family member could get TB. This is because it is caused by a bacteria which is transmitted through the air via talking, singing and coughing, so anyone can breathe it in – as was the situation (and therefore, panic) with Covid. The mode of transmission is the main similarity between TB and COVID-19 – there are lots of differences.
While some people are more at risk of getting TB, anyone can get TB, from any background. As a recent example: in 2024 Anna (name changed), a professional woman who lived in a green leafy suburb, was referred to me by her GP. Anna was shocked and outraged that she had been diagnosed with TB: “Janet, I feel as if I have been infected with a third world plague”. Anna wanted to believe that she had been infected with TB on a visit to India 18 months previously, but together we traced back her potential exposure and worked out she most likely was infected six months earlier, by a family member in a care home. Because Anna and her GP did not think about TB, it took more than a month of her coughing, losing weight and having no energy and taking several courses of antibiotics, before the diagnosis was finally made. By this time, she was very unwell, and her family members and many clients were at risk of getting TB.
Anna’s experience highlights how stigmatised TB still is as a disease. Stigma is a challenge to people from all backgrounds, and there are different reasons for it. Talking about TB more openly is one way to reduce stigma.
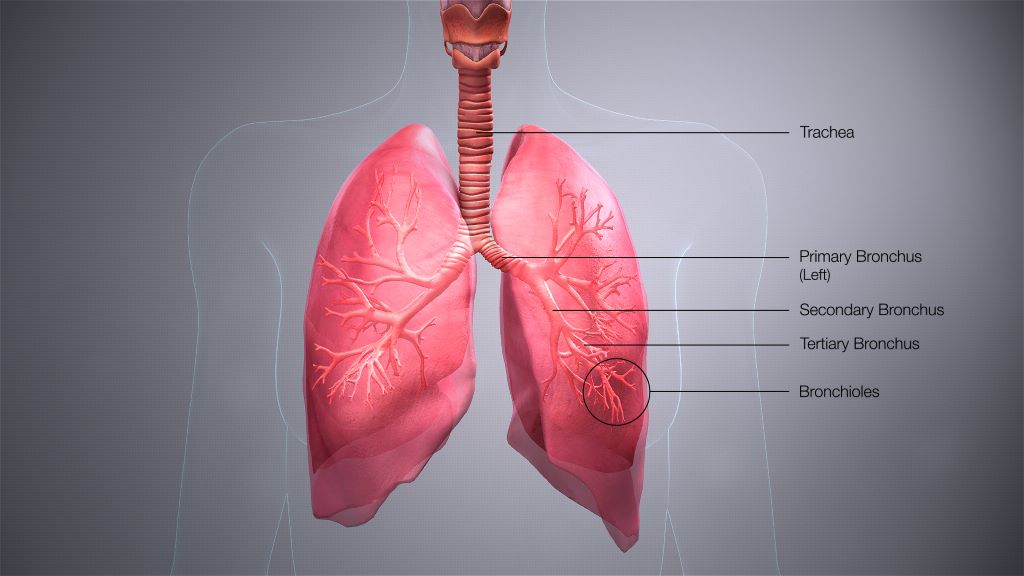
As with many other diseases, the earlier TB is diagnosed, the better the chance of full recovery, with no residual lung damage. There is effective medication to treat TB, and although treatment typically takes 6 months, it is not lifelong unlike chronic diseases like diabetes, hypertension and HIV. Young children with uncomplicated lung TB take medication for 4 months only.
Recent TB guidelines recommend that all close contacts of people diagnosed with TB (usually family or household members) should be tested for TB (even if they don’t have symptoms), and if they test negative, they can be offered TB preventive treatment (TPT), which will protect them against getting active TB disease. There is also more “user friendly” TPT now available, which consists of taking medication once a week for 3 months – a total of 12 doses only. Counselling people with TB needs to be family focused, given these new developments.
So, my challenge to readers is to have regular intentional conversations about TB with family and friends, with colleagues, in airplanes, and while waiting in queues.
Keely, a young women who read a previous Spotlight article I wrote, said she was amazed to discover that her colleague was very anxious because her mother was being treated for TB. If Keely had not decided to talk about TB at work, she would not have been able to offer her colleague support.
Try having a conversation about TB in the next week and see what comes of it.
*Giddy is a consultant at the TB advocacy group TB Proof.
Note: Spotlight aims to deepen public understanding of important health issues by publishing a variety of views on its opinion pages. The views expressed in this article are not necessarily shared by the Spotlight editors.
Republished from Spotlight under a Creative Commons licence.
Read the original article.