Surprising Drug Duo Outperforms Oseltamivir in Treating Flu

In a potential game-changer for how we treat the flu, scientists at the Hebrew University of Jerusalem have unveiled a new drug pairing that outperforms oseltamivir – the most widely used anti-influenza medication – against even the deadliest flu strains, including bird(avian) and swine flu.
The surprising duo? One of them is theobromine, a compound found in chocolate.
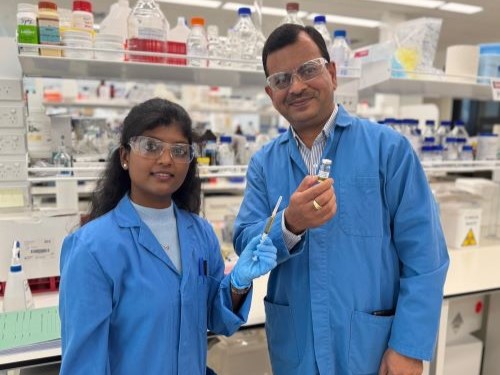
In a study recently published in PNAS, researchers, led by Prof Isaiah (Shy) Arkin, have developed a novel combination therapy that targets a key weakness in the influenza virus: its ion channel, a microscopic gate the virus uses to replicate and spread. By blocking this gate, the team effectively cut off the virus’s ability to survive.
Their study, conducted at Israel’s new Barry Skolnick Biosafety Level 3 facility, tested this combo, consisting of theobromine and a lesser-known compound called arainosine, against a broad range of flu viruses. In both cell cultures and animal trials, the treatment dramatically outperformed oseltamivir (Tamiflu), especially against drug-resistant strains.
“We’re not just offering a better flu drug,” said Prof Arkin. “We’re introducing a new way to target viruses – one that may help us prepare for future pandemics.”
Why It Matters
The stakes are high: Influenza continues to sweep the globe each year, with unpredictable mutations that challenge vaccines and existing drugs. In the U.S. alone, seasonal flu costs an estimated $87 billion annually in healthcare and lost productivity. Past pandemics – like the 2009 swine flu – have inflicted even deeper global costs, and the cost of future pandemics was estimated to rise even further up to $4.4 trillion.
Meanwhile, outbreaks of avian flu have devastated poultry industries and sparked fears of cross-species transmission to humans. Just one recent outbreak in the U.S. led to the loss of 40 million birds and billions in economic damage.
Current flu treatments, like oseltamivir, are losing ground as the virus adapts. Most drugs in use target a viral protein that mutates frequently, rendering treatments less effective over time. That’s where Arkin’s team saw an opening.
A New Strategy for Old Viruses
Instead of fighting the virus head-on with traditional antivirals, the researchers zeroed in on the M2 ion channel – a crucial viral feature that helps the virus replicate. Past efforts to block this channel have largely failed due to drug resistance. But the new theobromine–arainosine combo sidesteps this resistance, even neutralising hard-to-treat strains.
The team discovered the combo by scanning a library of repurposed compounds, many originally developed for other diseases, and testing their effects on both drug-sensitive and drug-resistant versions of the virus.
Broader Implications
The implications extend beyond influenza. Because many viruses, including coronaviruses, also rely on ion channels, this new approach could form the basis of future antiviral strategies.
The next steps include human clinical trials, but the early results offer hope not just for a better flu treatment, but for a smarter way to fight viral disease in general. ViroBlock, a startup company emanating from the Hebrew University, has been entrusted to develop the discoveries to reach the public.
Source: Hebrew University of Jerusalem