Losing the Y Chromosome to Age Drives Bladder Cancers but Improves Immunotherapy

As men age, some of their cells lose their Y chromosome and this loss hampers the body’s ability to fight cancer, according to new research from Cedars-Sinai Cancer. The study, published in Nature, found that loss of the Y chromosome helps cancer cells evade the immune system, resulting in aggressive bladder cancer. Somehow, this also renders the disease more responsive to immune checkpoint inhibitors.
Based on their research, investigators are developing a test for loss of the Y chromosome in tumours with the goal of helping clinicians tailor immune checkpoint inhibitor treatment for male patients with bladder cancer.
“This study for the first time makes a connection that has never been made before between loss of the Y chromosome and the immune system’s response to cancer,” said corresponding author Dan Theodorescu, MD, PhD, who initiated the research. “We discovered that loss of the Y chromosome allows bladder cancer cells to elude the immune system and grow very aggressively.”
Lead collaborators on the study also included Johanna Schafer, a postdoctoral fellow, and Zihai Li, MD, PhD, medical oncologist and immunologist, both at The Ohio State University Comprehensive Cancer Center-James Cancer Hospital and Solove Research Institute.
In men, loss of the Y chromosome has been observed in several cancer types, including 10%–40% of bladder cancers. Loss of the Y chromosome also has been associated with heart disease and Alzheimer’s disease.
The Y chromosome contains the blueprints for certain genes. Based on the way these genes are expressed in normal cells in the bladder lining, investigators developed a scoring system to measure loss of the Y chromosome in cancers.
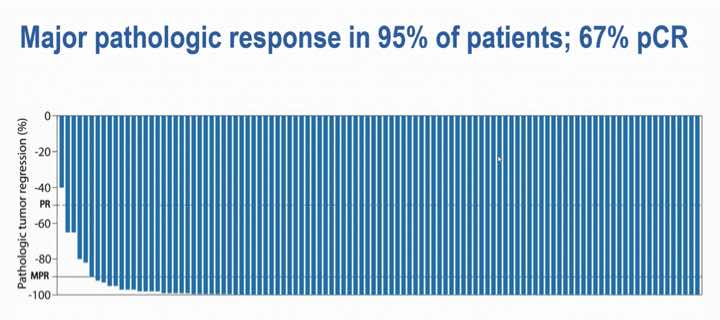
The investigators then reviewed data on two groups of men. One group had muscle invasive bladder cancer and had their bladders removed, but were not treated with an immune checkpoint inhibitor. The other group participated in a clinical trial and were treated with an immune checkpoint inhibitor. They found that patients with loss of the Y chromosome had poorer prognosis in the first group and much better overall survival rates in the latter.
To determine why this happens, investigators next compared growth rates of bladder cancer cells from laboratory mice.
Cancer cells were grown in vitro and not exposed to immune cells. The researchers also grew the diseased cells in mice that were missing T-cells. In both cases, tumours with and without the Y chromosome grew at the same rate.
In mice with intact immune systems, tumours lacking the Y chromosome grew at a much faster rate than did tumours with the intact Y chromosome.
“The fact that we only see a difference in growth rate when the immune system is in play is the key to the ‘loss-of-Y’ effect in bladder cancer,” Theodorescu said. “These results imply that when cells lose the Y chromosome, they exhaust T-cells. And without T-cells to fight the cancer, the tumor grows aggressively.”
Based on their results derived from human patients and laboratory mice, Theodorescu and his team also concluded that tumours missing the Y chromosome, while more aggressive, were also more vulnerable and responsive to immune checkpoint inhibitors. This therapy, one of the two mainstay bladder cancer treatments available to patients today, reverses T-cell exhaustion and allows the body’s immune system to fight the cancer.
“Fortunately, this aggressive cancer has an Achilles’ heel, in that it is more sensitive than cancers with an intact Y chromosome to immune checkpoint inhibitors,” said co-first author Hany Abdel-Hafiz, PhD, associate professor at Cedars-Sinai Cancer.
Preliminary data not yet published shows that loss of the Y chromosome also renders prostate cancers more aggressive, Theodorescu said.
“Our investigators postulate that loss of the Y chromosome is an adaptive strategy that tumour cells have developed to evade the immune system and survive in multiple organs,” said Shlomo Melmed, MB, ChB, dean of the Medical Faculty at Cedars-Sinai. “This exciting advance adds to our basic understanding of cancer biology and could have far-reaching implications for cancer treatment going forward.”
Further work is needed to help investigators understand the genetic connection between loss of the Y chromosome and T-cell exhaustion.
“If we could understand those mechanics, we could prevent T-cell exhaustion,” Theodorescu said. “T-cell exhaustion can be partially reversed with checkpoint inhibitors, but if we could stop it from happening in the first place, there is much potential to improve outcomes for patients.”
While women do not have a Y chromosome, Theodorescu said these findings could have implications for them as well. The Y chromosome contains a set of related genes, called paralogue genes, on the X chromosome, and these might play a role in both women and in men. Additional research is needed to determine what that role might be.
“Awareness of the significance of Y chromosome loss will stimulate discussions about the importance of considering sex as a variable in all scientific research in human biology,” Theodorescu said. “The fundamental new knowledge we provide here may explain why certain cancers are worse in either men or women, and how best to treat them. It also illustrates that the Y chromosome does more than determine human biologic sex.”
Source: Cedars-Sinai Medical Center