New Laser System Measures Scalp and Brain Blood Flow
This optical measurement could offer an affordable and scalable way to diagnose stroke, brain injury and other conditions
Measuring blood flow in the brain is critical for responding to a range of neurological problems, including stroke, traumatic brain injury (TBI) and vascular dementia. But existing techniques, including magnetic resonance imaging and computed tomography, are expensive and therefore not widely available.
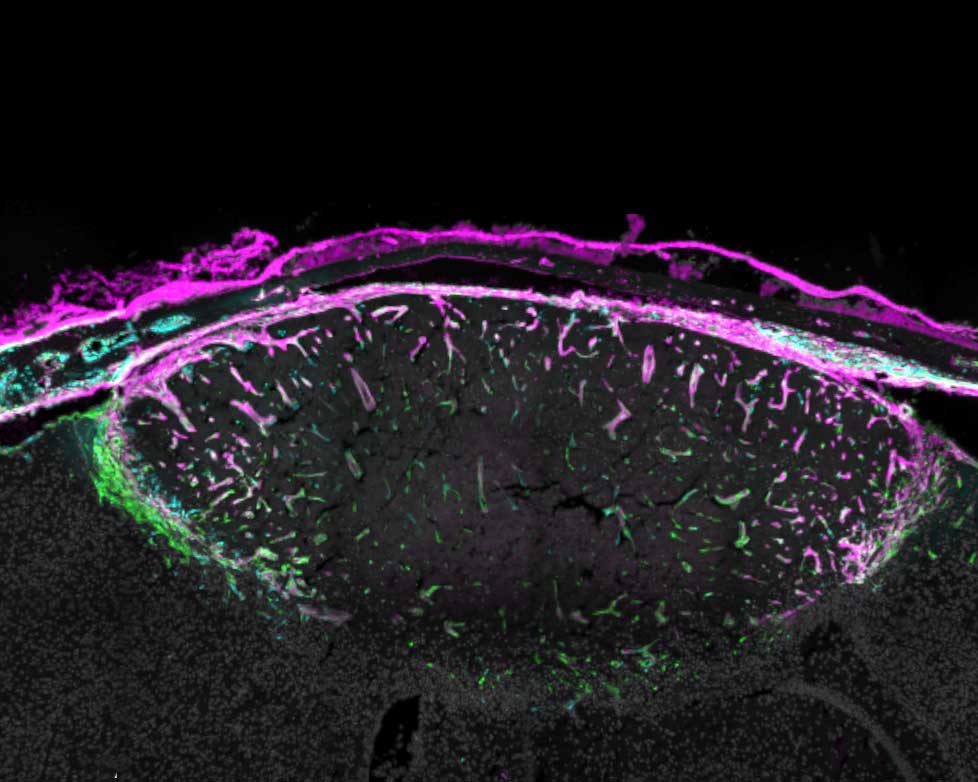
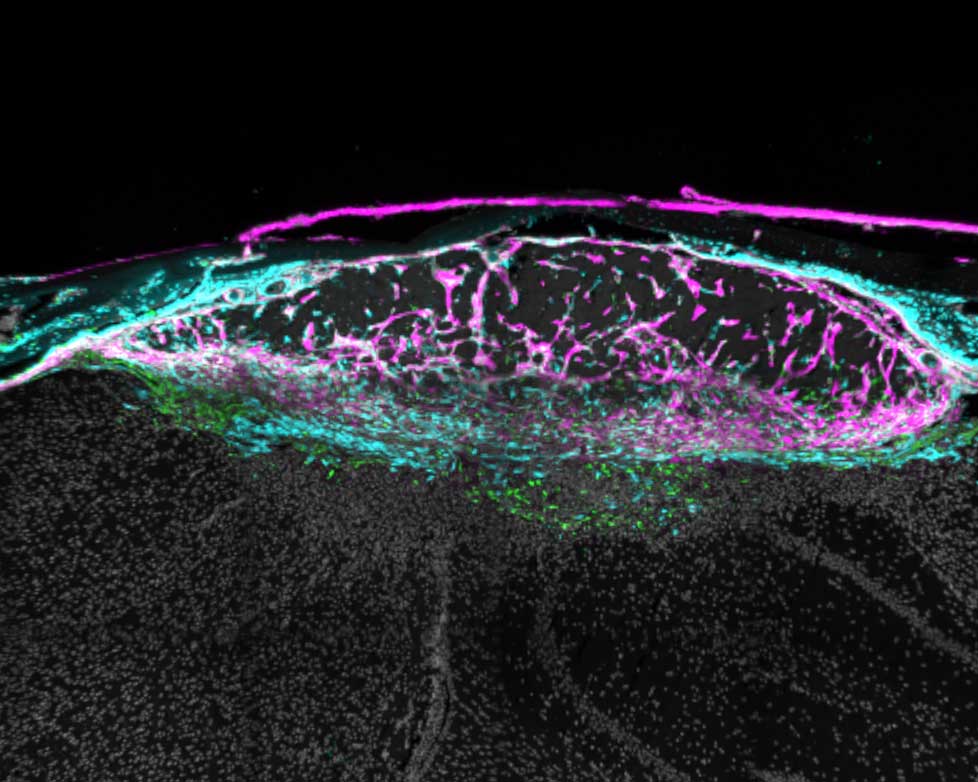
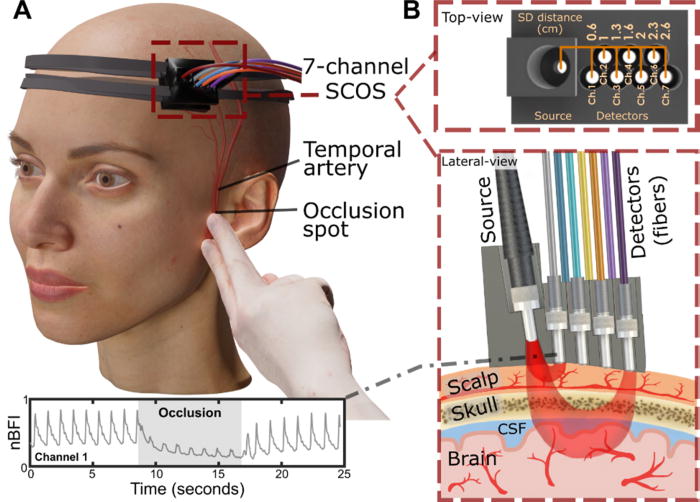
Researchers from the USC Neurorestoration Center and the California Institute of Technology (Caltech) have built a simple, noninvasive alternative. The device takes a technique currently used in animal studies known as speckle contrast optical spectroscopy (SCOS) and adapts it for potential clinical use in humans. It works by capturing images of scattered laser light with an affordable, high-resolution camera.
“It’s really that simple. Tiny blood cells pass through a laser beam, and the way the light scatters allows us to measure blood flow and volume in the brain,” said Charles Liu, MD, PhD, professor of clinical neurological surgery, urology and surgery at the Keck School of Medicine of USC, director of the USC Neurorestoration Center and co-senior author of the new research.
The device has already been tested with humans in small proof of concept studies demonstrating the tool’s utility for assessing stroke risk and detecting brain injury. In the current study, published in APL Bioengineering, Liu and his team sought to confirm that SCOS is truly measuring blood flow in the brain, rather than in the scalp, which also contains many blood vessels. The question has long plagued researchers who use light-based technology to visualize the brain.
Liu’s team took an innovative approach: By temporarily blocking blood flow to the scalp, they confirmed that SCOS readings were indeed measuring signals from blood vessels in the brain. Readings from 20 participants showed that positioning the detector at least 2.3cm away from the laser source provided the clearest measurement of brain blood flow. The study, funded in part by the National Institutes of Health, the Alfred Mann Foundation and the USC Neurorestoration Center, was just published in the journal APL Bioengineering.
“For the first time in humans, this experimental evidence shows that a laser speckle optical device can probe beyond the scalp layers to access cerebral signals,” said Simon Mahler, PhD, who is now an assistant professor in the Department of Biomedical Engineering at the Stevens Institute of Technology and one of the paper’s coauthors. “This is an important step toward using SCOS to non-invasively measure blood flow in the brain.”
Tracking brain blood flow
For years, researchers measuring brain signals with light-based technology, such as lasers and fibre optics, have used statistical simulations to estimate which signals originate in the brain versus the scalp. The USC Neurorestoration Center team found a direct way to test the difference, thanks to a collaboration between surgeons, engineers and neurologists.
“I perform surgeries to increase blood flow in the brain, and many of these involve temporarily stopping blood flow in the scalp,” said Jonathan Russin, MD, now professor and chief of neurosurgery at the University of Vermont, who continues to collaborate with the USC Neurorestoration Center. “That gave us a simple way to test the technology – by creating a change that affected only the scalp’s circulation while leaving the brain’s blood flow untouched.”
In 20 participants, the researchers temporarily stopped blood flow to the scalp, then collected a series of SCOS readings. By gradually moving the detector further from the head, they captured signals reaching progressively deeper towards the brain. They found that positioning the detector 2.3cm from the head allowed them to measure brain blood flow while minimising interference from the scalp.
The findings confirm the utility of SCOS for non-invasively detecting brain blood flow and provide important guidance for other researchers working with light-based technology, Liu said.
Bringing SCOS to patients
Beyond advancing research, the study helps confirm the clinical potential of SCOS for detecting and responding to stroke, brain injury and dementia. Because all of the team’s research has been done with humans, the tool is poised for rapid translation from the lab to the clinic.
“We look directly at humans in essentially the same way the tool will be applied, so there’s nothing lost in translation,” Liu said. “We are never more than one step away from the problem we’re trying to solve.”
The technique is already being used by some of the team’s collaborators to help diagnose stroke and TBI. Next, the researchers will continue to refine the technology and software, working to improve the resolution of images and the quality of data extracted from readings.
“With the knowledge that we’re now measuring exactly what we intend to measure, we’re also going to expand our testing of this technique with patients in clinical settings,” Liu said.
Source: Keck School of Medicine of USC