Antioxidants Boost Tumour Growth by Stimulating Blood Vessel Formation

A new study from Karolinska Institutet shows that vitamin C and other antioxidants stimulate the formation of new blood vessels in lung cancer tumours. Published in The Journal of Clinical Investigation, this discovery corroborates the idea that dietary supplements containing antioxidants can accelerate tumour growth and metastasis.
“We’ve found that antioxidants activate a mechanism that causes cancer tumours to form new blood vessels, which is surprising, since it was previously thought that antioxidants have a protective effect,” says study leader Martin Bergö, professor and vice president of Karolinska Institutet in Sweden. “The new blood vessels nourish the tumours and can help them grow and spread.”
Antioxidants neutralise free oxygen radicals, which can damage the body, and are therefore commonly found in dietary supplements. But overly high doses can be harmful.
“There’s no need to fear antioxidants in normal food but most people don’t need additional amounts of them,” says Professor Bergö. “In fact, it can be harmful for cancer patients and people with an elevated cancer risk.”
Previously unknown mechanism
Professor Bergö’s research group has previously shown that antioxidants like vitamin C and E accelerate the growth and spread of lung cancer by stabilising a protein called BACH1. BACH1 is activated when the level of free oxygen radicals drops, which happens, for example, when extra antioxidants are introduced via the diet or when spontaneous mutations in the tumour cells activate endogenous antioxidants. Now the researchers have been able to show that the activation of BACH1 induces angiogenesis, the formation of new blood vessels .
While hypoxia is known to be required for angiogenesis to occur in cancer tumours, the new mechanism identified by the researchers demonstrates that tumours can form new blood vessels in the presence of normal oxygen levels as well. The study also shows that BACH1 is regulated in a similar way as the HIF-1α protein – a mechanism that was awarded the 2019 Nobel Prize in Physiology or Medicine and that allows cells to adapt to changes in oxygen levels. HIF-1α and BACH1 work together in the tumours, the new research shows.
Hoping for more effective drugs
“Many clinical trials have evaluated the efficacy of angiogenesis inhibitors, but the results have not been as successful as anticipated,” says Ting Wang, doctoral student in Professor Bergö’s group at Karolinska Institutet. “Our study opens the door to more effective ways of preventing angiogenesis in tumours; for example, patients whose tumours exhibit high levels of BACH1 might benefit more from anti-angiogensis therapy than patients with low BACH1 levels.”
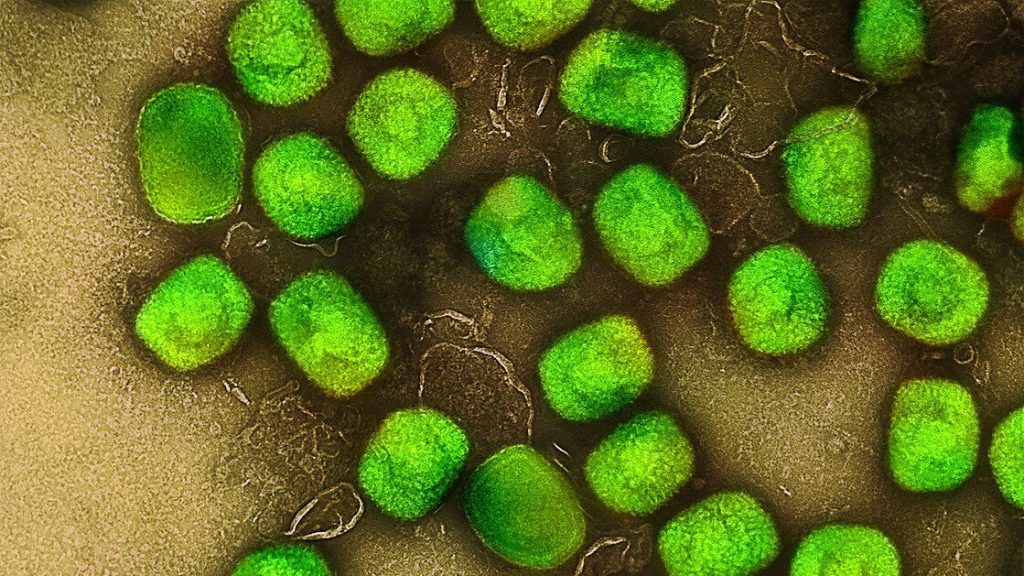
The researchers used a range of cell-biological methods and concentrated most of their work on lung cancer tumours by studying organoids, as well as mice and samples of human breast and kidney tumours. Tumours in which BACH1 was activated, either via ingested antioxidants or by overexpression of the BACH1 gene, produced more new blood vessels and were highly sensitive to angiogenesis inhibitors.
“The next step is to examine in detail how levels of oxygen and free radicals can regulate the BACH1 protein, and we will continue to determine the clinical relevance of our results,” says Ting Wang. “We’ll also be doing similar studies in other cancer forms such as breast, kidney and skin cancer.”
Source: Karolinska Institute