Are Ultra-processed Foods the New ‘Silent Killer’?

Nowadays, ultra-processed foods are packed with a bewildering range of additives: there are common ones like oil, fat, and sugar. There are also emulsifiers such as carrageenan, mono- and diglycerides, carboxymethylcellulose, polysorbate and soy lecithin. These continue to strip food of healthy nutrients while introducing other ingredients that could also be detrimental to human health.
Hundreds of novel ingredients never encountered by human physiology are now found in nearly 60% of the average adult’s diet and nearly 70% of children’s diets in the United States.
While obesity and lack of physical activity are well recognised contributors to avoidable morbidity and mortality, another emerging hazard is the unprecedented consumption of these ultra-processed foods in the standard American diet. This may be the new “silent” killer, as was unrecognised hypertension in previous decades.
Physicians from Florida Atlantic University’s Schmidt College of Medicine explored this hypothesis and provide important insights to health care providers in a battle where the entertainment industry, the food industry and public policy do not align with their patients’ needs. Their findings are published in a commentary in The American Journal of Medicine.
First generation of doctors to see a reduction in life expectancy
“Those of us practicing medicine in the US today find ourselves in an ignominious and unique position – we are the first cohort of health care professionals to have presided over a decline in life expectancy in 100 years,” said Dawn H. Sherling, MD, corresponding author, associate program director for the internal medicine residency and an associate professor of medicine, FAU Schmidt College of Medicine. “Our life expectancy is lower than other economically comparable countries. When we look at increasing rates of non-communicable diseases in less developed nations, we can see a tracking of this increase along with increasing consumption of ultra-processed foods in their diets.”
Although professional organizations such as the American College of Cardiology cautions patients to “choose minimally processed foods instead of ultra-processed foods” in their 2021 dietary guidelines, there is a caveat that “there is no commonly accepted definition for ultra-processed foods, and some healthy foods may exist within the ultra-processed food category.”
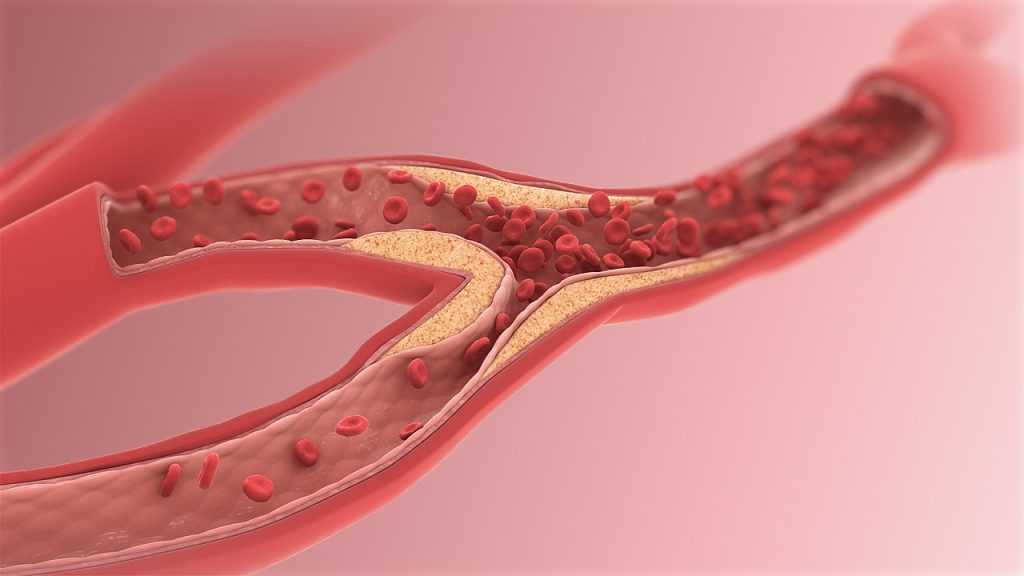
“When the components of a food are contained within a natural, whole food matrix, they are digested more slowly and more inefficiently, resulting in less calorie extraction, lower glycaemic loads in general, and lower rise in triglyceride-rich lipoproteins after eating, which could result in atherosclerotic plaque,” said Allison H. Ferris, MD, senior author, an associate professor and chair, Department of Medicine, and director of the internal medicine residency program, FAU Schmidt College of Medicine. “Therefore, even if the troublesome additives were removed from the ultra-processed food, there would still be concern for an over-consumption of these products possibly leading to obesity, diabetes and heart disease.”
The authors add that public health organisations are increasingly making use of the NOVA classification system, which divides foods into four categories – whole foods, culinary ingredients (items like butter, oil and salt), traditionally processed foods (such as bread and yogurt made with few ingredients), and ultra-processed foods – or those foods that are industrially made and use ingredients not normally found in a domestic kitchen.
According to the authors, one plausible mechanism to explain the hazards is that ultra-processed foods contain emulsifiers and other additives that the mammalian gastrointestinal tract mostly does not digest. They may act as a food source for our microbiota, and as such may be creating a dysbiotic microbiome that can, in the right host, promote disease.
“Additives, such as maltodextrin, may promote a mucous layer that is friendly to certain species of bacteria that are found in greater abundance in patients with inflammatory bowel disease,” said Sherling. “When the mucous layer is not properly maintained, the epithelial cell layer may become vulnerable to injury, as has been shown in feeding studies using carrageenan in humans and other studies in mice models, using polysorbate-80 and cellulose gum, triggering immunologic responses in the host.”
Food companies as powerful as the 20th century’s tobacco companies
The authors add that there have been marked increases in colorectal cancer in the US, especially among younger adults. They opine that increased ultra-processed food consumption may be a contributor as well as to several other gastrointestinal diseases.
“Whether ultra-processed foods contribute to our currently rising rates of non-communicable disease requires direct testing in analytic studies designed a priori to do so,” said Charles H. Hennekens, MD, FACPM, co-author, the First Sir Richard Doll Professor of Medicine and senior academic advisor, FAU Schmidt College of Medicine. “In the meantime, we believe it is incumbent upon all health care professionals to discuss the benefits of increasing consumption of whole foods and reducing consumption of ultra-processed foods with their patients.”
The authors also opine that just as the dangers of tobacco began to emerge during the middle of the prior century, decades passed before the preponderance of the evidence and the efforts of forward-thinking health officials prompted policy change to discourage the use of cigarettes. They say there is likely to be a similar path for ultra-processed foods.
“The multinational companies that produce ultra-processed foods are just as, if not more, powerful than tobacco companies were in the last century, and it is unlikely that governments will be able to move quickly on policies that will promote whole foods and discourage the consumption of ultra-processed foods,” said Sherling. “Importantly, health care providers also should remain cognizant of the difficulties that many of our patients have in being able to afford and find healthier options, which calls for a broader public health response.”
Source: Florida Atlantic University