Food Allergies may Protect Some against COVID

A recent study in the journal Frontiers in Immunology may explain why some cases of COVID are asymptomatic: common foods, vaccines, bacteria and viruses may all prime the immune system to attack SARS-CoV-2 due to bearing similar antigens to the virus. The study paves the way for new immunotherapies or vaccines that lead to stronger immunity against COVID.
Proteins present in bacteria, human cells, vaccines, and even foods may all share similarities with those in SARS-CoV-2. The researchers behind this latest study hypothesised that similarities between SARS-CoV-2 and other common proteins may affect our susceptibility to the virus.
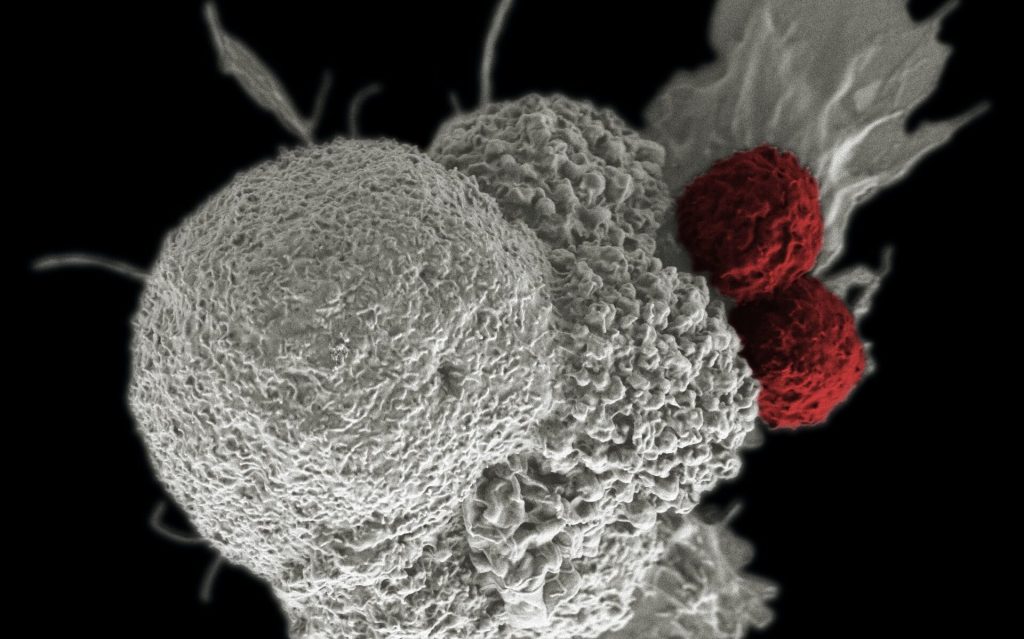
After the initial infection by a pathogen has passed, T and B cells retain a memory of it, ready to rapidly produce more antibodies if needed. Food allergies are a result of the immune system targeting the proteins in what are otherwise harmless substances.
Testing antibody cross-reactions
Could such an ‘immune memory’ to proteins we have encountered in our past underlie immune resistance and reduced susceptibility to Covid-19? To begin to test this hypothesis, these researchers investigated whether antibodies that target proteins in the SARS-CoV-2 virus could also bind to proteins in other agents, such as foods or common bacteria.
The researchers tested the ability of these antibodies to bind to 180 different proteins from common foods, two different vaccines, and 15 bacterial and viral proteins. The antibodies reacted most strongly with a common gut bacterium called E. faecalis and a vaccine against diphtheria, tetanus, and pertussis. Interestingly, they also reacted very strongly against proteins found in common foods, including broccoli, roasted almonds, pork, cashews, milk, soy, and pineapple.
Eat for immunity?
Unfortunately, you will likely not be able to eat your way to COVID immunity. ‘Immunity’ against a food type, for instance, is typically characterised by a food allergy. “Usually only people with leaky gut can make antibodies against food, so I wouldn’t actually recommend eating foods that give you leaky gut, because this would give you a whole new set of problems,” said Dr Aristo Vodjani of Cyrex Laboratories in Arizona, lead author on the study.
Indeed, the researchers caution that although these agents could potentially provide some protection from SARS-CoV-2, they are no replacement for current vaccines. Further studies are also needed to confirm that these proteins do indeed confer some protection, and if so, whether it is mediated through a short-lived antibody response or a longer-term memory cell response.
The findings may shed some light on our variable responses to COVID infection. With more research, these results could lead to more effective treatments or better vaccines against the virus. Another application may lie in assessing an individual’s susceptibility to the virus before they have even been infected.
Source: EurekAlert!