Paediatric Kidney Transplants without Immunosuppressive Drugs

Stanford Medicine physicians have developed a way to provide paediatric kidney transplants without immunosuppressive drugs. Their key innovation is a safe method to transplant the donor’s immune system to the patient before surgeons implant the kidney.
The medical team has dubbed the two-transplant combination a “dual immune/solid organ transplant,” or DISOT. The first three DISOT cases, all performed at Lucile Packard Children’s Hospital Stanford were described in the New England Journal of Medicine, accompanied by an an editorial about the research.
The Stanford innovation removes the possibility that the recipient will experience immune rejection of their transplanted organ, the most common reason for a second organ transplant The new procedure also rids recipients of the substantial side effects of a lifetime of immune-suppressing medications, including increased risks for cancer, diabetes, infections and hypertension.
“Safely freeing patients from lifelong immunosuppression after a kidney transplant is possible.”
Alice Bertaina, MD, PhD, report’s lead author, associate professor of paediatrics, Stanford University
The first three DISOT patients were children with a rare immune disease, but the team is expanding the types of patients who could benefit. The protocol received FDA approval on May 27, 2022, for treating patients with a variety of conditions that affect the kidneys. Dr Bertaina anticipates that the protocol will eventually be available to many people needing kidney transplants, starting with children and young adults, and later expanding to older adults. The researchers also plan to investigate DISOT’s utility for other types of solid-organ transplants.
The scientific innovation from Dr Bertaina’s team has another important benefit: It enables safe transplantation between a donor and recipient whose immune systems are genetically half-matched, meaning children can receive stem cell and kidney donations from a parent.
The advance is especially meaningful for Jessica and Kyle Davenport of Muscle Shoals, Alabama. Their two children, both born with a rare and potentially deadly immune disease, are among the first recipients of DISOT: 8-year-old Kruz received transplants from Jessica, while his 7-year-old sister, Paizlee, received transplants from Kyle.
“They’ve healed and recovered, and are doing things we never thought would be possible,” said Jessica Davenport. After years of helping Kruz and Paizlee cope with severe immune deficiency and its attendant infection riskk as well as kidney dialysis, she and her husband are thrilled that their children have more normal lives.
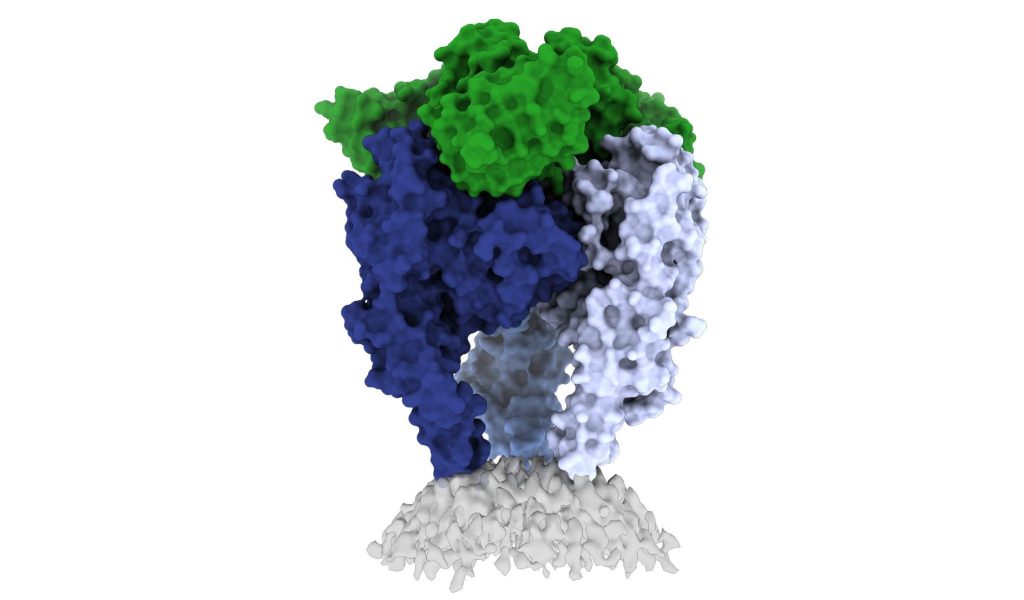
The idea of transplanting a patient with their organ donor’s immune system has been around for decades, but it has been difficult to implement. Transplants of stem cells from bone marrow provide the patient with a genetically new immune system, as some of the bone marrow stem cells mature into immune cells in the blood. First developed for people with blood cancers, stem cell transplants carry the risk of the new immune cells attacking the recipient’s body, a potentially lethal complication called graft-versus-host disease.
Source: Stanford Medicine