BCG Vaccine Activates Immune System in Newborns
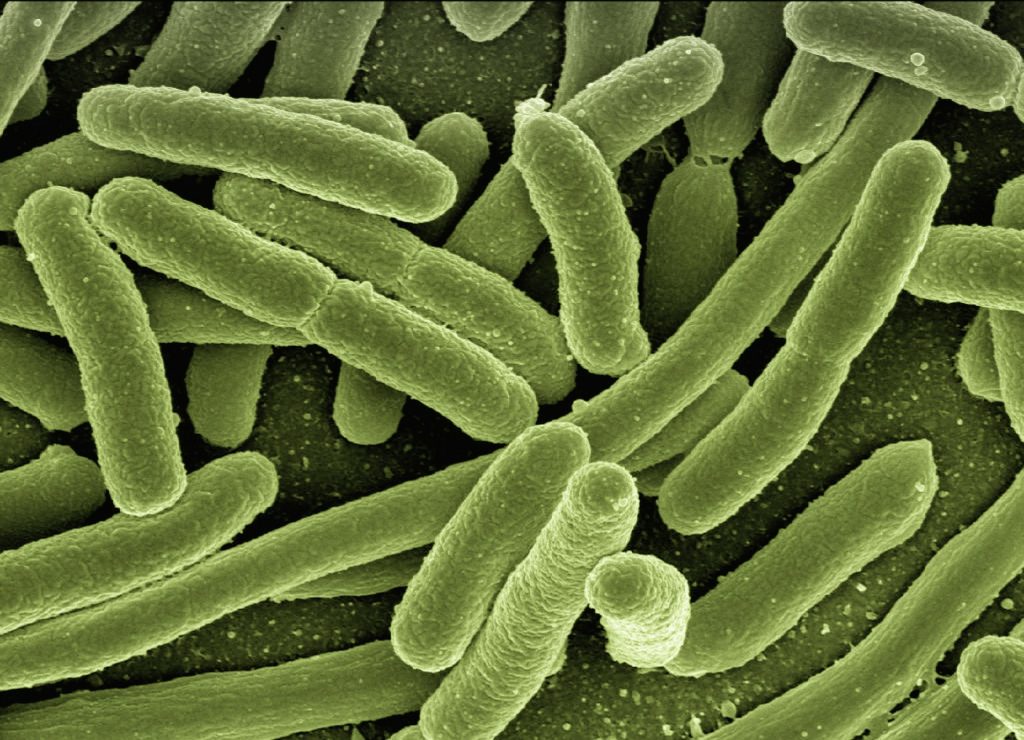
In the century since it was first used in humans, the Bacille Calmette-Guérin (BCG) vaccine against tuberculosis has become one of the world’s most widely used vaccines. Administered in countries with endemic TB, it has surprisingly been found to protect newborns and young infants against multiple bacterial and viral infections unrelated to TB. Some evidence even suggests that it can reduce severity of COVID. Now, a new study in Cell Reports sheds light on the mechanisms behind its extra protective effects.
Surprisingly little is known about how BCG exerts its many side benefits. To better understand its mechanism of action, researchers collected and comprehensively profile blood samples from newborns vaccinated with BCG, using a powerful ‘big data’ approach analysing lipid and metabolite biomarkers.
Their study found that the BCG vaccine induces specific changes in metabolites and lipids that correlate with innate immune system responses. The findings provide clues toward making other vaccines more effective in vulnerable populations with distinct immune systems, such as newborns.
First author Dr Joann Diray Arce and her colleagues started off with blood samples from low-birthweight newborns in Guinea Bissau who were enrolled in a randomised clinical trial to receive BCG either at birth or after a delay of six weeks. Blood samples were taken at four weeks for both groups (after BCG was given to the first group, and before it was given to the second group).
The researchers comprehensively profiled the impact of BCG immunisation on the newborns’ blood plasma. They found that BCG vaccines given at birth changed metabolite and lipid profiles in newborns’ blood plasma in a pattern distinct from those in the delayed-vaccine group. The changes were associated with changes in cytokine production, a key feature of innate immunity.
The researchers had parallel findings when they tested BCG in cord blood samples from a cohort of Boston newborns and samples from a separate study of newborns in The Gambia and Papua New Guinea.
“We now have some lipid and metabolic biomarkers of vaccine protection that we can test and manipulate in mouse models,” said Dr Arce. “We studied three different BCG formulations and showed that they converge on similar pathways of interest. Reshaping of the metabolome by BCG may contribute to the molecular mechanisms of a newborn’s immune response.”
“A growing number of studies show that BCG vaccine protects against unrelated infections,” said Ofer Levy, MD, PhD, the study’s senior investigator. “It’s critical that we learn from BCG to better understand how to protect newborns. BCG is an ‘old school’ vaccine – it’s made from a live, weakened germ – but live vaccines like BCG seem to activate the immune system in a very different way in early life, providing broad protection against a range of bacterial and viral infections. There’s much work ahead to better understand that and use that information to build better vaccines for infants.”
Source: Boston Children’s Hospital via News-Medical.Net