Why Drugs Targeting Interleukin-17 Don’t Work in Rheumatoid Arthritis
Cedars-Sinai investigators may have figured out why certain immunosuppressive treatments don’t work well in rheumatoid arthritis. In a study published in Science Immunology, scientists traced the problem to specific changes that occur in immune cells within the joints as the disease progresses.
The findings could lead to more effective therapies for the incurable autoimmune disease.
“Our discoveries point to the importance of the tissue environment in worsening rheumatoid arthritis and driving resistance to antirheumatic medications,” said Nunzio Bottini, MD, PhD, director of the Kao Autoimmunity Institute at Cedars-Sinai, professor of Medicine and corresponding author of the study.
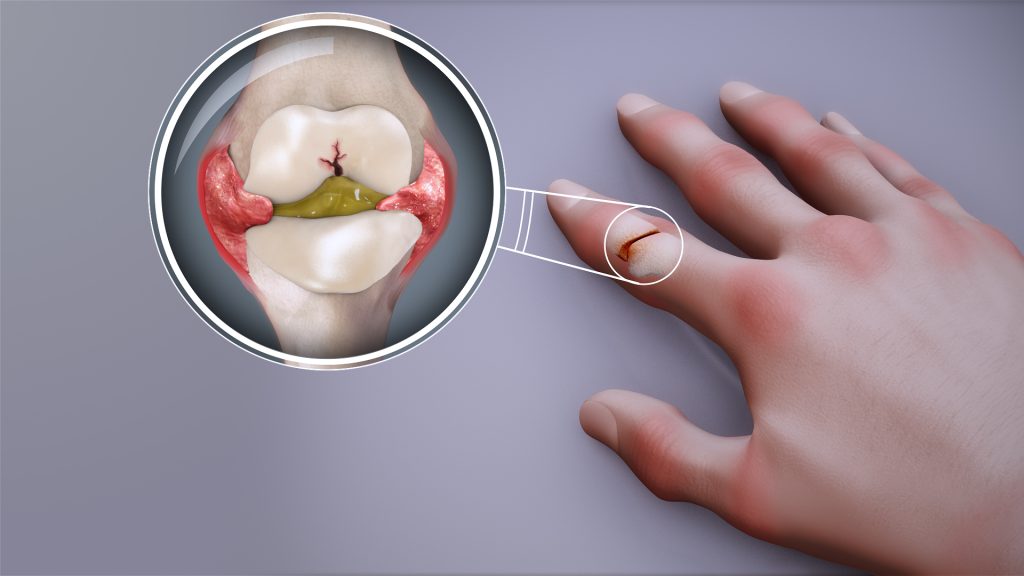
Rheumatoid arthritis causes chronic inflammation in the joints. In other forms of autoimmune arthritis, inflammation can be relieved by targeting interleukin-17, one of several proteins that can contribute to joint inflammation.
In experiments involving human rheumatoid arthritis tissues and laboratory mice, investigators showed that, over time, the immune cells that produce interleukin-17 gradually stop making it. This finding helps explain why IL-17-targeted treatments do not work well against established rheumatoid arthritis.
“These immune cells can also change in ways that make them more aggressive and able to sustain inflammation even without interleukin-17,” Bottini said.
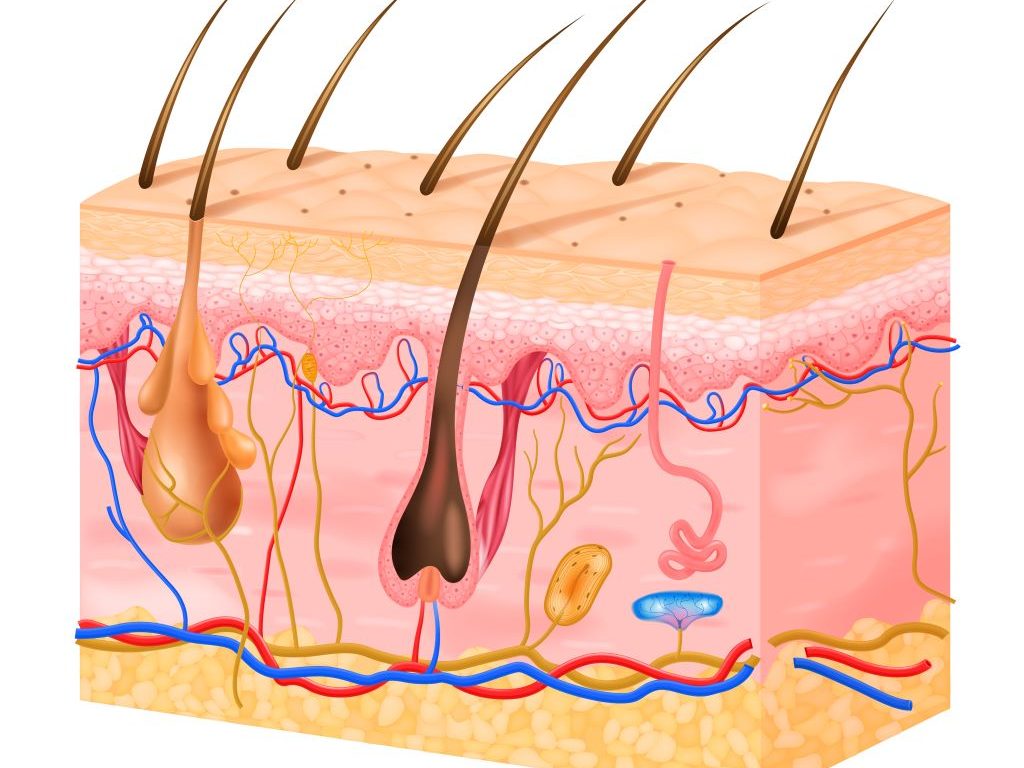
Changes to the immune cells appear to be driven by synoviocytes – nonimmune cells that produce the lubricating synovial fluid in the joints, according to the study.
Bottini said that the Department of Computational Biomedicine at Cedars-Sinai, particularly the laboratory of Kyoung Jae Won, PhD, played a key role in the study by contributing critical work in spatial biology, an emerging field that studies how cells function within their tissue environments.
The findings carry significant implications for treating rheumatoid arthritis, according to Joyce So, MD, PhD, chief genomics officer at Cedars-Sinai and medical director of the newly established Center for Genomic Medicine at Cedars-Sinai Guerin Children’s.
“This important new insight contributes to shifting the paradigm of how we understand rheumatoid arthritis progression and why IL-17 treatments haven’t worked as well as expected,” So said. “Only with a precise understanding of the biological mechanisms of disease can effective, precision therapies be developed. In the meantime, clinicians can help patients in early or presymptomatic stages make the most of treatments that may lose effectiveness over time.”
Source: Cedars–Sinai