Quitting Smoking Late in Life May Still Slow Cognitive Decline

Quitting smoking in middle age or later is linked to slower age-related cognitive decline over the long term, according to a new study by UCL researchers.
The study, published in The Lancet Healthy Longevity, looked at data from 9436 people aged 40 or over (average age: 58) in 12 countries, comparing cognitive test results among people who quit smoking with those of a matched control group who kept smoking.
The research team found that the cognitive scores of those who had quit smoking declined significantly less than their smoking counterparts in the six years after they quit. For verbal fluency, the rate of decline roughly halved, while for memory it slowed by 20%.
Since slower cognitive decline is related to reduced dementia risk, their findings add to a growing body of evidence suggesting quitting smoking might be a preventative strategy for the disease. Still, more research is needed to confirm this.
Lead author Dr Mikaela Bloomberg (UCL Institute of Epidemiology & Health Care) said: “Our study suggests that quitting smoking may help people to maintain better cognitive health over the long term even when we are in our 50s or older when we quit.
“We already know that quitting smoking, even later in life, is often followed by improvements in physical health and well-being. It seems that, for our cognitive health too, it is never too late to quit.
“This finding is especially important because middle-aged and older smokers are less likely to try to quit than younger groups, yet they disproportionately experience the harms of smoking. Evidence that quitting may support cognitive health could offer new compelling motivation for this group to try and quit smoking.
“Also, as policymakers wrestle with the challenges of an ageing population, these findings provide another reason to invest in tobacco control.”
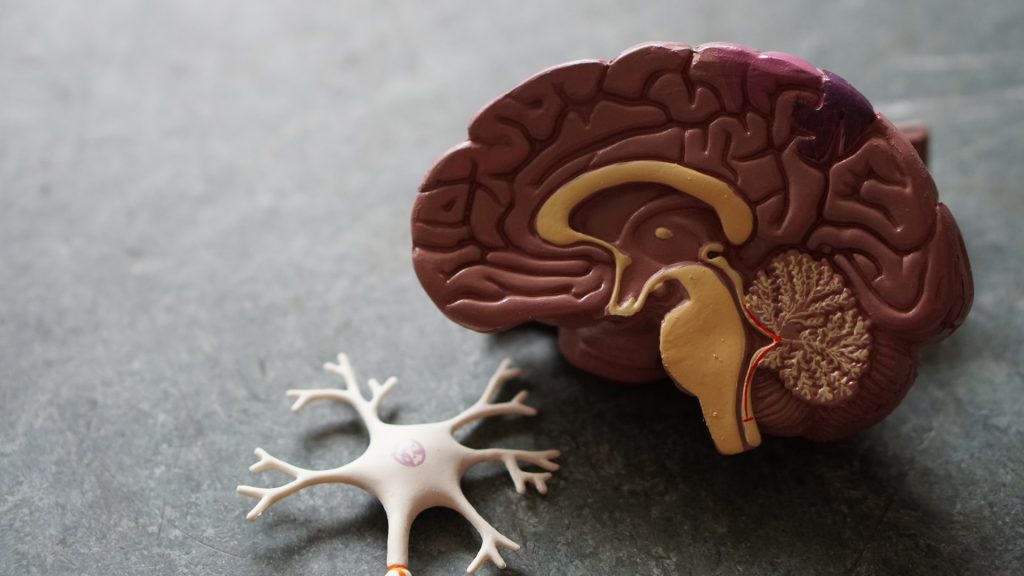
Smoking is thought to harm brain health in part because it affects cardiovascular health – smoking causes damage to blood vessels that supply oxygen to the brain. Smoking is also thought to affect cognitive health by causing chronic inflammation and directly damaging brain cells through oxidative stress (due to the creation of unstable molecules called free radicals).
Co-author Professor Andrew Steptoe (UCL Institute of Epidemiology & Health Care) said: “Slower cognitive decline is linked to lower dementia risk. These findings add to evidence suggesting that quitting smoking might be a preventative strategy for the disease. However, further research will be needed that specifically examines dementia to confirm this.”
Previous studies, the researchers noted, had found a short-term improvement in cognitive function after people stopped smoking. But whether this improvement was sustained over the longer term – particularly when people quit smoking later in life – was not known.
To answer this question the research team looked at data from three ongoing studies* where a nationally representative group of participants answered survey questions every two years. The studies covered England, the US, and 10 other European countries.
More than 4,700 participants who quit smoking were compared with an equal number of people who carried on smoking. The two groups were matched in terms of their initial cognitive scores and other factors such as age, sex, education level, and country of birth.
The research team found that the two groups’ scores in memory and verbal fluency tests declined at a similar rate in the six years prior to participants of one group quitting smoking. These trajectories then diverged in the six years following smoking cessation.
For the smokers who quit, the rate of decline was about 20% slower for memory and 50% slower for verbal fluency. In practical terms, this meant that with each year of ageing, people who quit experienced three to four months less memory decline and six months less fluency decline than those who continued smoking.
This was an observational analysis, so unmeasured differences between smokers who quit and continuing smokers could remain; while the trends before quitting were similar, the study cannot prove cause and effect.
However, the research team noted their findings were consistent with earlier studies showing that adults aged over 65 who quit smoking during early- or mid-life have comparable cognitive scores to never smokers, and that former and never smokers have a similar risk of dementia a decade or longer after quitting.
*The longitudinal studies were the English Longitudinal Study of Ageing (ELSA), the Survey of Health, Ageing and Retirement in Europe (SHARE), and the Health and Retirement Study (HRS).
Source: University College London