Pocket Ultrasound Reduces Hospital Stays for Patients with Shortness of Breath

When hospitalised patients struggle to breathe, doctors typically reach for their stethoscopes, but results from a clinical study in JAMA Network Open suggest they should diagnose the problem with portable ultrasounds instead.
The study, by Rutgers Universitty and RWJBarnabas Health, found initial exams with portable ultrasounds led to better diagnoses, shorter hospital stays and big cost savings. However, the findings revealed a need for additional training and workflow integration to help clinicians transition from traditional tools to this promising new technology.
“The study clearly shows that ultrasound is the superior diagnostic technology, even for long-time stethoscope users who get a few hours of ultrasound training,” said senior study author Partho Sengupta, Henry Rutgers professor and chief of cardiology at Rutgers Robert Wood Johnson Medical School (RWJMS), chief of cardiology at Robert Wood Johnson University Hospital (RWJUH) and member of the RWJBarnabas Health Medical Group.
The explanation here is simple. Ultrasound gives you more information, and more concrete information, about what’s going on
Partho Sengupta, Henry Rutgers professor
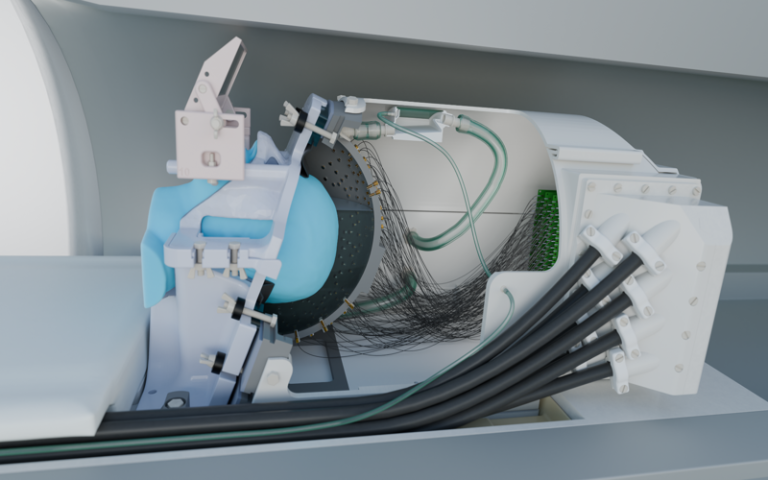
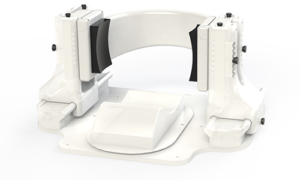
The study enrolled 208 patients admitted with shortness of breath to Robert Wood Johnson University Hospital in New Brunswick. About half of them underwent diagnosis via point-of-care ultrasound devices that attach to smartphones. The rest underwent diagnosis via existing standards of care.
Initial diagnosis with ultrasound trimmed a patient’s average length of hospital stay from 11.9 days to 8.3 days. In all, initial diagnosis with ultrasound saved 246 bed-days and about $751 000 in direct costs across the cohort, while 30-day readmissions were similar between groups.
“The explanation here is simple. Ultrasound gives you more information, and more concrete information, about what’s going on,” Sengupta said. “When clinicians can see fluid in the lungs, a failing heart or a stiff inferior vena cava in minutes, they can target therapy sooner or rule out a cardiopulmonary cause and look elsewhere.”
To keep things simple and encourage buy-in, scans focused on a handful of cardiac views and a six-zone lung sweep. The exam was designed to be quick and binary: signs of congestion or not, systolic function reduced or not.
The study provided several hours of ultrasound training to participating hospitalists (doctors who oversee and coordinate hospital patient care) so that each could perform and interpret the ultrasound exam in 10 to 15 minutes.
Nevertheless, most hospitalists who underwent the training let sonographers perform the exams and cardiologists interpret them. Only 20% of patients received an ultrasound diagnosis from one of the hospitalists.
Sengupta said time pressure on rounds and a lack of incentives make it hard to add a 10-minute procedure, even if it changes care.
“This is consistent with what we observe in day-to-day clinical practice,” Sengupta said. “Although the ultrasound probe fits in your pocket and attaches to the back of a smartphone, its use in clinical settings remains inconsistent. This study overcame those barriers by leveraging a multidisciplinary framework.”
Kameswari Maganti, professor of cardiology at RWJMS and section chief for non-invasive cardiology at RWJUH, led the image interpretation with the sonography team that worked closely with the RWJUH hospitalist team, led by RWJMS faculty Catherine Chen and Payal Parikh, as well as the engineering and data science team, headed by Naveena Yanamala.
“This coordinated team effort was key to developing and delivering a streamlined protocol that significantly reduced hospital stays and healthcare costs,” Sengupta said.
The researchers reported that ultrasound findings altered medical decisions in roughly a third of cases, including new diagnoses and changes in therapy. They also noted that longer-stay patients appeared to benefit the most, a hint that ultrasound-guided triage and treatment may pay particular dividends when cases are complex.
As with most single-center implementations, caveats apply. The model relied on trained sonographers and cardiology reads, which may not be available everywhere. Broader studies across multiple hospitals will be needed to confirm the cost and length-of-stay benefits, and to test strategies that make adoption stick.
Still, the argument for seeing more and guessing less is gaining ground. A bedside view of the heart and lungs, delivered early in admission, may help the right treatments arrive sooner.
Source: Rutgers University