Iron Plays a Major Role in Down Syndrome-Associated Alzheimer’s Disease
New USC research indicates how iron-related oxidative damage and cell death may hasten the development of Alzheimer’s disease in people with Down syndrome

Scientists at the University of Southern Carolina have discovered a key connection between high levels of iron in the brain and increased cell damage in people who have both Down syndrome and Alzheimer’s disease.
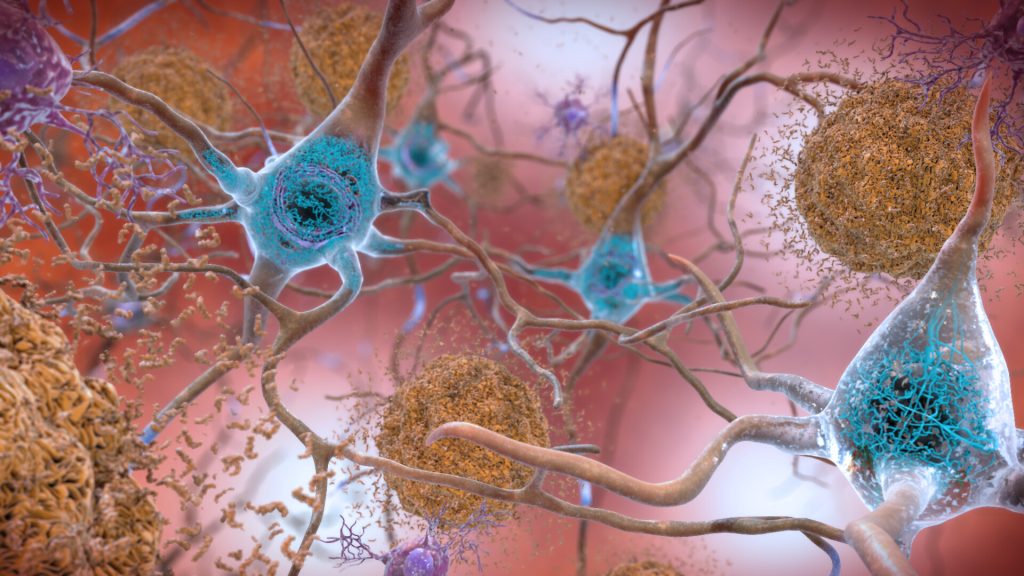
In the study, researchers found that the brains of people diagnosed with Down syndrome and Alzheimer’s disease (DSAD) had twice as much iron and more signs of oxidative damage in cell membranes compared to the brains of individuals with Alzheimer’s disease alone or those with neither diagnosis. The results, published in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, point to a specific cellular death process that is mediated by iron, and the findings may help explain why Alzheimer’s symptoms often appear earlier and more severely in individuals with Down syndrome.
“This is a major clue that helps explain the unique and early changes we see in the brains of people with Down syndrome who develop Alzheimer’s,” said Max Thorwald, lead author of the study and a postdoctoral fellow in the laboratory of University Professor Emeritus Caleb Finch at the USC Leonard Davis School. “We’ve known for a long time that people with Down syndrome are more likely to develop Alzheimer’s disease, but now we’re beginning to understand how increased iron in the brain might be making things worse.”
Down syndrome and Alzheimer’s
Down syndrome is caused by having an extra third copy, or trisomy, of chromosome 21. This chromosome includes the gene for amyloid precursor protein, or APP, which is involved in the production of amyloid-beta (Aβ), the sticky protein that forms telltale plaques in the brains of people with Alzheimer’s disease.
Because people with Down syndrome have three copies of the APP gene instead of two, they tend to produce more of this protein. By the age of 60, about half of all people with Down syndrome show signs of Alzheimer’s disease, which is approximately 20 years earlier than in the general population.
“This makes understanding the biology of Down syndrome incredibly important for Alzheimer’s research,” said Finch, the study’s senior author.
Key findings point to ferroptosis
The research team studied donated brain tissue from individuals with Alzheimer’s, DSAD, and those without either diagnosis. They focused on the prefrontal cortex — an area of the brain involved in thinking, planning, and memory — and made several important discoveries:
- Iron levels much higher in DSAD brains: Compared to the other groups, DSAD brains had twice the amount of iron in the prefrontal cortex. Scientists believe this buildup comes from tiny brain blood vessel leaks called microbleeds, which occur more frequently in DSAD than in Alzheimer’s and are correlated with higher amounts of APP.
- More damage to lipid-rich cell membranes: Cell membranes are made of fatty compounds called lipids and can be easily damaged by chemical stress. In DSAD brains, the team found more byproducts of this type of damage, known as lipid peroxidation, compared to amounts in Alzheimer’s-only or control brains.
- Weakened antioxidant defense systems: The team found that the activity of several key enzymes that protect the brain from oxidative damage and repair cell membranes was lower in DSAD brains, especially in areas of the cell membrane called lipid rafts.
Together, these findings indicate increased ferroptosis, a type of cell death characterised by iron-dependent lipid peroxidation, Thorwald explained: “Essentially, iron builds up, drives the oxidation that damages cell membranes, and overwhelms the cell’s ability to protect itself.”
Lipid rafts: a hotspot for brain changes
The researchers paid close attention to lipid rafts — tiny parts of the brain cell membrane that play crucial roles in cell signalling and regulate how proteins like APP are processed. They found that in DSAD brains, lipid rafts had much more oxidative damage and fewer protective enzymes compared to Alzheimer’s or healthy brains.
Notably, these lipid rafts also showed increased activity of the enzyme β-secretase, which interacts with APP to produce Aβ proteins. The combination of more damage and more Aβ production may promote the growth of amyloid plaques, thus speeding up Alzheimer’s progression in people with Down syndrome, Finch explained.
Rare Down syndrome variants offer insight
The researchers also studied rare cases of individuals with “mosaic” or “partial” Down syndrome, in which the third copy of chromosome 21 is only present in a smaller subset of the body’s cells. These individuals had lower levels of APP and iron in their brains and tended to live longer. In contrast, people with full trisomy 21 and DSAD had shorter lifespans and higher levels of brain damage.
“These cases really support the idea that the amount of APP — and the iron that comes with it — matters a lot in how the disease progresses,” Finch said.
Looking ahead
The team says their findings could help guide future treatments, especially for people with Down syndrome who are at high risk of Alzheimer’s. Early research in mice suggests that iron-chelating treatments, in which medicine binds to the metal ions and allows them to leave the body, may reduce indicators of Alzheimer’s pathology, Thorwald noted.
“Medications that remove iron from the brain or help strengthen antioxidant systems might offer new hope,” Thorwald said. “We’re now seeing how important it is to treat not just the amyloid plaques themselves but also the factors that may be hastening the development of those plaques.”