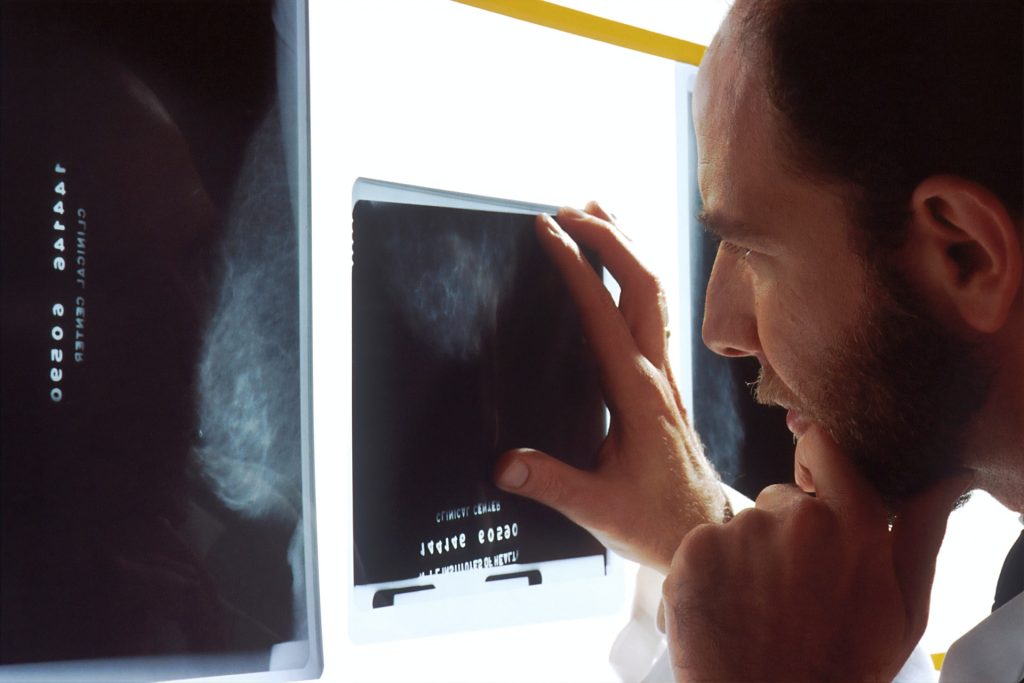
How Accurate is Supplemental Ultrasound in Breast Cancer Screening Failures?

Dense breast tissue, which contains a higher proportion of fibrous tissue than fat, is a risk factor for breast cancer and also makes it more difficult to identify cancer on a mammogram. Many US states have enacted laws that require women with dense breasts to be notified after a mammogram, so that they can choose to undergo supplemental ultrasound screening to improve cancer detection. A recent study published by Wiley online in CANCER, a peer-reviewed journal of the American Cancer Society, evaluated the results of such additional screening to determine its benefits and harms to patients.
Although supplemental ultrasound screening may detect breast cancers missed by mammography, it requires additional imaging and may lead to unnecessary breast biopsies among women who do not have breast cancer. Therefore, it is important to use supplemental ultrasound only in women at high risk of mammography screening failure – in other words, women who develop breast cancer after a mammogram shows no signs of malignancy.
Brian Sprague, PhD, of the University of Vermont Cancer Center, and his colleagues evaluated 38 166 supplemental ultrasounds and 825 360 screening mammograms without supplemental ultrasounds during 2014–2020 at 32 US imaging facilities within three regional registries of the Breast Cancer Surveillance Consortium.
The team found that 95.3% of supplemental ultrasounds were performed in women with dense breasts. In comparison, 41.8% of mammograms without additional screening were performed in women with dense breasts.
Among women with dense breasts, a high risk of interval invasive breast cancer was present in 23.7% of women who underwent ultrasounds, compared with 18.5% of women who had mammograms without additional imaging.
The findings indicate that ultrasound screening was highly targeted to women with dense breasts, but only a modest proportion of these women were at high risk of mammography screening failure. A similar proportion of women who received only mammograms were at high risk of mammography screening failure.
“Among women with dense breasts, there was very little targeting of ultrasound screening to women who were at the highest risk of a mammography screening failure. Rather, women with dense breasts undergoing ultrasound screening had similar risk profiles to women undergoing mammography screening alone,” said Dr Sprague. “In other words, many women at low risk of breast cancer despite having dense breasts underwent ultrasound screening, while many other women at high risk of breast cancer underwent mammography alone with no supplemental screening.”
Clinicians can consider other breast cancer risk factors beyond breast density to identify women who may be appropriate for supplemental ultrasound screening. Publicly available risk calculators from the Breast Cancer Surveillance Consortium are available that also consider age, family history, and other factors (https://www.bcsc-research.org/tools).
Source: Wiley