Researchers Discover that Lupus is Triggered by Epstein-Barr Virus

Epstein-Barr virus (EBV) one, of humanity’s most ubiquitous infectious pathogens, is to blame for systemic lupus erythematosus Stanford Medicine investigators and their colleagues have found.
The Epstein-Barr virus (EBV), which resides silently inside 95% of the world’s population, is directly responsible for making a minuscule number of immune cells go rogue and persuade far more of their fellow immune cells to launch a widespread assault on the body’s tissues, the scientists have shown.
The findings were published in Science Translational Medicine.
“This is the single most impactful finding to emerge from my lab in my entire career,” said William Robinson, MD, PhD, a professor of immunology and rheumatology and the study’s senior author. “We think it applies to 100% of lupus cases.”
The study’s lead author is Shady Younis, PhD, professor and instructor in immunology and rheumatology.
About five million worldwide – 90% of them women – have lupus in which the immune system attacks the contents of cell nuclei. This results in damage to organs and tissues throughout the body, with symptoms varying widely among individuals.
Practically the only way to not get EBV is to live in a bubble.”
With appropriate diagnosis and medication, most lupus patients can live reasonably normal lives, but for about 5% of them the disorder can be life-threatening, said Robinson,. Existing treatments slow down disease progression but don’t cure it, he said.
The virus meets the B cell
By the time we’ve reached adulthood, the vast majority of us have been infected by EBV. Transmitted in saliva, EBV infection typically occurs in childhood, from sharing a spoon with or drinking from the same glass as a sibling or a friend, or maybe during our teen years, from exchanging a kiss. EBV can cause mononucleosis, “the kissing disease,” which begins with a fever that subsides but lapses into a profound fatigue that can persist for months.
“Practically the only way to not get EBV is to live in a bubble,” Robinson said. “If you’ve lived a normal life,” the odds are nearly 20 to 1 you’ve got it.
Once you’ve been infected by EBV you can’t get rid of it, Robinson said, even if you remain or become symptom-free. EBV belongs to a large family of viruses, including those responsible for chickenpox and herpes, that can deposit their genetic material into the nuclei of infected cells. There the virus slumbers in a latent form, hiding from the immune system’s surveillance agents. This may last as long as the cell it’s hiding in stays alive. Or, under certain conditions, the virus may reactivate and force the infected cell’s replicative machinery to produce myriad copies of themselves that break out to infect other cells and other people.
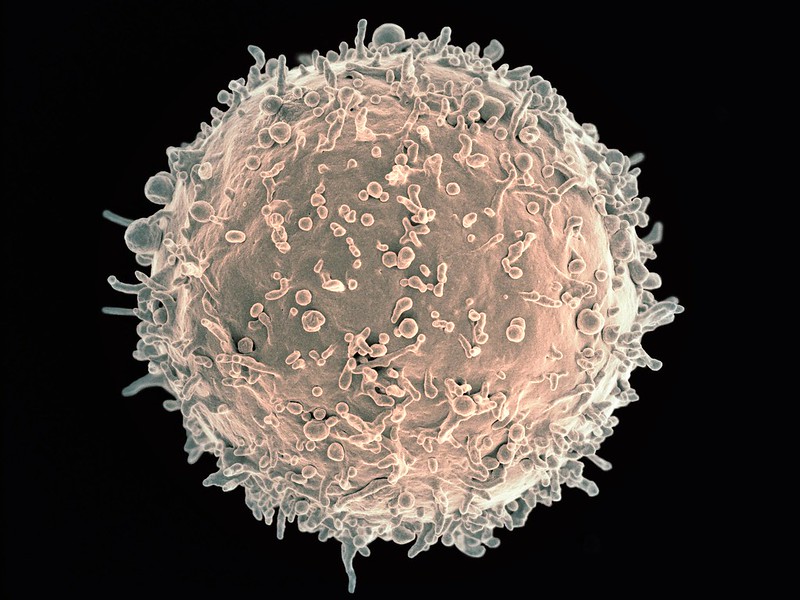
Among the cell types in which EBV takes up permanent residence are B cells, immune cells that do a couple of important things after they ingest bits of microbial pathogens. For one, they can produce antibodies: customised proteins that find and bind immune-system-arousing proteins or other molecules (immunologists call them “antigens”) on microbial pathogens that have infected an individual, or are trying to. For another, B cells are “professional antigen-presenting cells”: They can process antigens and display them on their surfaces to encourage other immune cells to raise the intensity of their hunt for the pathogen in question. That’s a substantial force multiplier for kick-starting an immune response.
Our bodies harbour hundreds of billions of B cells, which, through many cell divisions, develop an enormous diversity of antibodies. In the aggregate, these antibodies can bind an estimated 10 billion to 100 billion different antigenic shapes. This is why we’re able to mount a successful immune response to so many different pathogens.
Oddly, about 20% of the B cells in our bodies are autoreactive. They target antigens belonging to our own tissues – not by design, but due to the random way B-cell diversity comes about: through sloppy replication, apparently engineered by evolution to ensure diversification. Fortunately, these B cells are typically in a dopey state of inertia, and they pretty much leave our tissues alone.
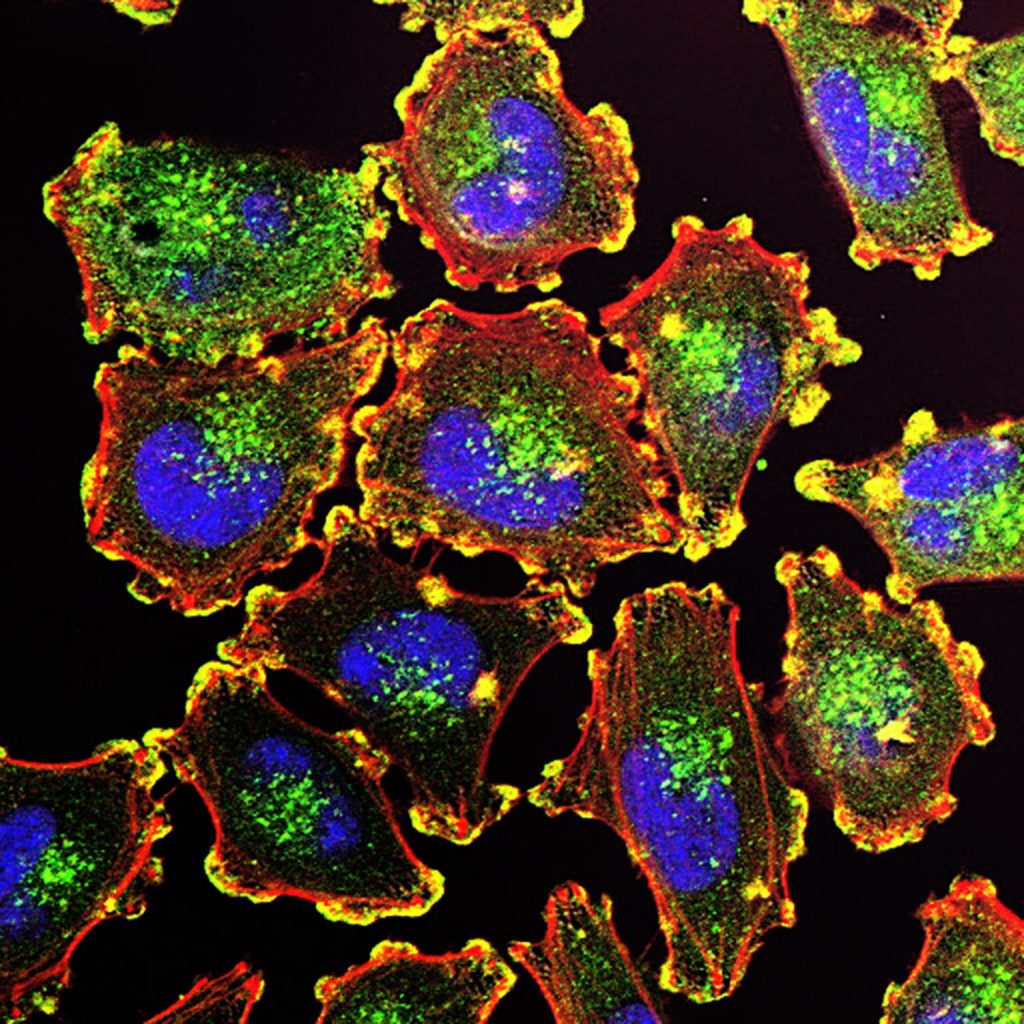
But at times, somnolent autoreactive B cells become activated, take aim at our own tissues and instigate one of the disorders collectively called autoimmunity. Some awakened autoreactive B cells crank out antibodies that bind to proteins and DNA inside the nuclei of our cells. Such activated “antinuclear antibodies” — the hallmark of lupus — trigger damage to tissues randomly distributed throughout the body, because virtually all our body’s cells have nuclei.
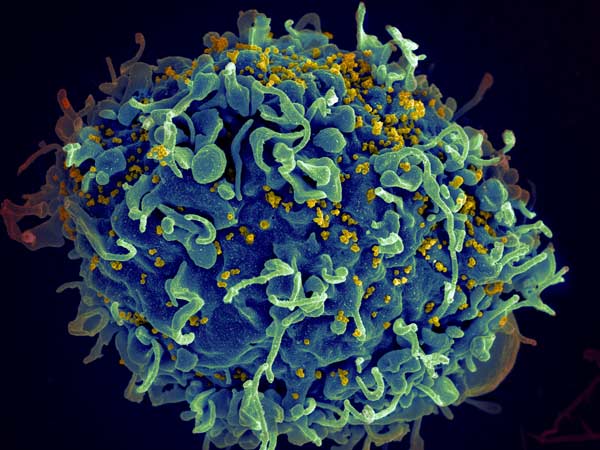
The vast majority of EBV-infected people (most of us, that is) have no idea they’re still sheltering a virus and never get lupus. But essentially everyone with lupus is EBV-infected, studies have shown. An EBV-lupus connection has been long suspected but never nailed down until now.
The antinuclear B cell gets ornery
Although latent EBV is ubiquitous in the sense that almost everybody carries it, it resides in only a tiny fraction of any given person’s B cells. As a result, until the new study, it was virtually impossible for existing methods to identify infected B cells and distinguish them from uninfected ones. But Robinson and his colleagues developed an extremely high-precision sequencing system that enabled them to do this. They found that fewer than 1 in 10,000 of a typical EBV-infected but otherwise healthy individual’s B cells are hosting a dormant EBV viral genome.
Employing their new EBV-infected-B-cell-identifying technology along with bioinformatics and cell-culture experimentation, the researchers found out how such small numbers of infected cells can cause a powerful immune attack on one’s own tissues. In lupus patients, the fraction of EBV-infected B cells rises to about 1 in 400 — a 25-fold difference.
It’s known that the latent EBV, despite its near-total inactivity, nonetheless occasionally nudges the B cell it’s been snoozing in to produce a single viral protein, EBNA2. The researchers showed that this protein acts as a molecular switch – a “transcription factor” – activating a battery of genes in the B cell’s genome that had previously been at rest. At least two of the human genes switched on by EBNA2 are recipes for proteins that are, themselves, transcription factors that turn on a variety of other pro-inflammatory human genes.
The net effect of all these genetic fireworks is that the B cell becomes highly inflammatory: It dons its “professional antigen-presenting cell” uniform and starts stimulating other immune cells (called helper T cells) that happen to share a predilection for targeting cell-nuclear components. These helper T cells enlist multitudes of other antinuclear B cells as well as antinuclear killer T cells, vicious attack dogs of the immune system.
When that militia bulks up, it doesn’t matter whether any of the newly recruited antinuclear B cells are EBV-infected or not. (The vast majority of them aren’t.) If there are enough of them, the result is a bout of lupus.
What comes next?
Robinson said he suspects that this cascade of EBV-generated self-targeting B-cell activation might extend beyond lupus to other autoimmune diseases such as multiple sclerosis, rheumatoid arthritis and Crohn’s disease, where hints of EBV-initiated EBNA2 activity have been observed.
The million-dollar question: If about 95% of us are walking around with latent EBV in our B cells, why do some of us, but not all of us, get autoimmunity? Robinson speculates that perhaps only certain EBV strains spur the transformation of infected B cells into antigen-presenting “driver” cells that broadly activate huge numbers of antinuclear B cells.
Many companies are working on an EBV vaccine, and clinical trials of such a vaccine are underway. But that vaccine would have to be given soon after birth, Robinson noted, as such vaccines are unable to rid an already-infected person of the virus.
Stanford University’s Office of Technology Licensing has filed a provisional patent application on intellectual property associated with the study’s findings and technologies used to obtain them. Robinson, Younis and a third study co-author, Mahesh Pandit, PhD, a postdoctoral scholar in immunology and rheumatology, are named inventors on the application. They are co-founders and stockholders of a company, EBVio Inc., a company exploring an experimental lupus treatment, ultradeep B-cell depletion. This procedure involves total annihilation of all circulating B cells, which are replaced over the following few months by new, EBV-free B cells born continually in the bone marrow. Robinson is also a director of EBVio Inc. and a co-founder and shareholder of Flatiron Bio, LLC.
Source: Stanford Medicine