Stem Cell Therapy Linked to Lower Risk of Heart Failure After a Heart Attack
Technique may be a valuable add-on procedure for patients with weak heart function after a heart attack, say researchers
Patients with weak heart function who receive stem cell therapy shortly after a heart attack are at lower risk of developing heart failure and related hospital stays compared with standard care, finds a clinical trial published by The BMJ.
The researchers say the findings suggest this technique may be a valuable add-on procedure for this particular group of patients after a heart attack to prevent subsequent heart failure and reduce the risk of future adverse events.
Advances in heart attack management have improved survival rates considerably, but this has also led to rising rates of subsequent heart failure. While recent studies have indicated that stem cell therapy may reduce rates of heart failure after a heart attack, clinical trials are needed to confirm these benefits.
To address this gap, the researchers set out to assess the impact of delivering stem cells directly into coronary arteries (known as intracoronary infusion) after a heart attack on the development of heart failure over three years.
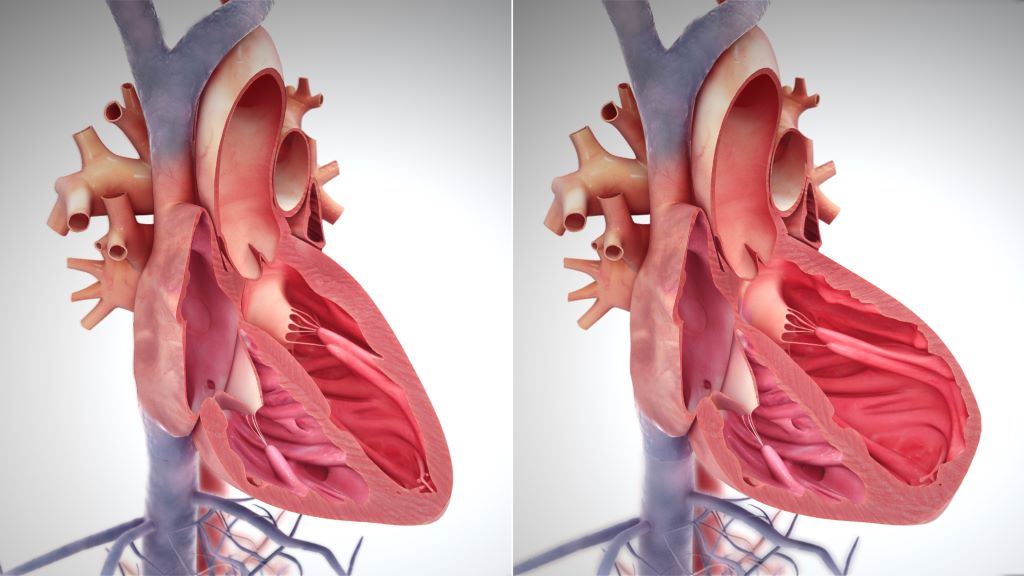
Their findings are based on 396 patients (average age 57-59 years) with no previous heart conditions at three teaching hospitals in Iran. They had all experienced a first heart attack (myocardial infarction) leading to extensive heart muscle damage and weakened heart function – where the left ventricle, the heart’s main pumping chamber, is too weak to pump blood out to the body as effectively as it should.
Of these, 136 patients in the intervention group received an intracoronary infusion of allogenic Wharton’s jelly derived mesenchymal stem cells within 3-7 days of their heart attack in addition to standard care. The remaining 260 control group patients received standard care alone.
Factors such as age, sex, baseline heart function, smoking status, obesity, existing high blood pressure, diabetes, or kidney problems were taken into account, and patients were monitored for an average of 33 months.
Compared with the control group, intracoronary infusion of stem cells was associated with reduced rates of heart failure (2.77 vs 6.48 per 100 person years), readmission to hospital for heart failure (0.92 vs 4.20 per 100 person years), and a combined measure of cardiovascular death and readmission for heart attack or heart failure (2.8 vs 7.16 per 100 person years).
The intervention did not have a statistically significant effect on readmission to hospital for heart attack (1.23 vs 3.06 per 100 person years), death from any cause (1.81 vs 1.66 per 100 person years), or cardiovascular death (0.91 vs 1.33 per 100 person-years).
However, by six months heart function in the intervention group showed a significantly greater improvement from baseline at six months compared with the control group.
This was a large trial with long term follow-up and clinically meaningful outcome measures, but the researchers acknowledge several limitations to their findings. These include the inability to do a sham procedure for the control group, which would have allowed for a double blinded study design instead of a single blinded format. Nor did they assess heart failure biomarkers or investigate the physiological effects of the intervention on heart tissue.
Nevertheless, they say these results suggest that this technique “may serve as a valuable adjunctive procedure after myocardial infarction to prevent the development of heart failure and reduce the risk of future adverse events.”
Additional trials confirming this finding are needed as well as further research “to explore the underlying mechanisms of mesenchymal stem cells therapy and to optimise its application in clinical practice,” they add.
Source: BMJ Group





