Scientists Uncover the Brain Mechanisms that Distinguish Imagination from Reality

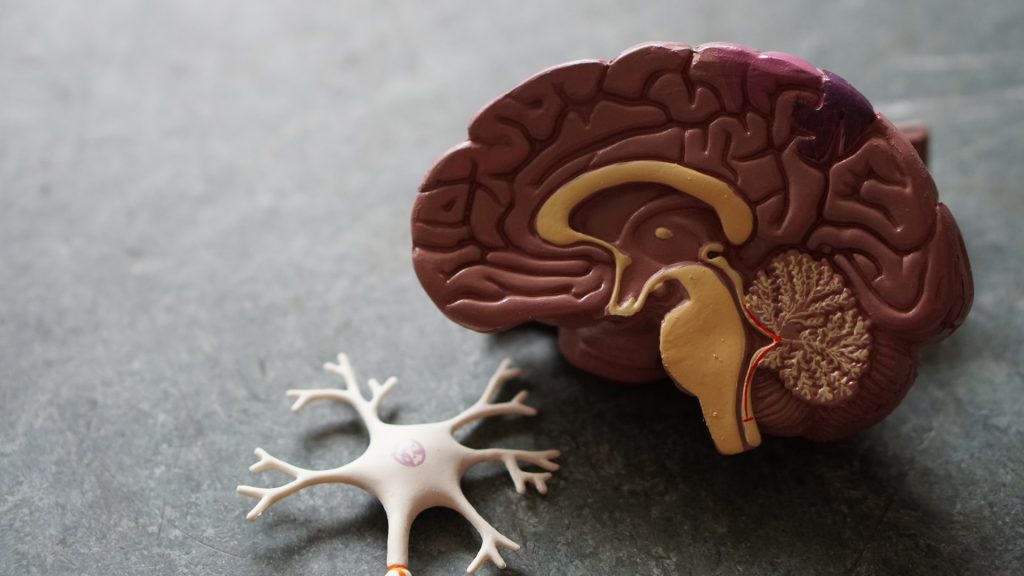
Areas of the brain that help a person differentiate between what is real and what is imaginary have been uncovered in a new study led by UCL researchers. The research, published in Neuron, found that a region in the brain known as the fusiform gyrus – located behind one’s temples, on the underside of the brain’s temporal lobe – is involved in helping the brain to determine whether what we see is from the external world or generated by our imagination.
The researchers hope that their findings will increase understanding of the cognitive processes that go awry when someone has difficulty judging what is real and what is not, such as in schizophrenia, and could eventually lead to advancement in diagnosing and treating these conditions.
Lead author, Dr Nadine Dijkstra (Department of Imaging Neuroscience at UCL) said: “Imagine an apple in your mind’s eye as vividly as you can. During imagination, many of the same brain regions activate in the same manner as when you see a real apple. Until recently, it remained unclear how the brain distinguishes between these real and imagined experiences.”
For the study, researchers asked 26 participants to look at simple visual patterns while imagining them at the same time.
Specifically, participants were asked to look for a specific faint pattern within a noisy background on a screen and indicate whether the pattern was actually present or not. A real pattern was only presented half of the time.
At the same time, participants were also instructed to imagine a pattern that was either the same or different to the one they were looking for, and indicate how vivid their mental images were.
When the patterns were the same, and participants reported that their imagination was very vivid, they were more likely to say they saw a real pattern, even on trials in which nothing was presented. This means they mistook their mental images for reality.
While participants performed the tasks, their brain activity was monitored using functional magnetic resonance imaging (fMRI). This technology enabled the researchers to identify which parts of the brain showed patterns of activity that helped distinguish reality from imagination.
The team found that the strength of activity in the fusiform gyrus could predict whether people judged an experience as real or imagined, irrespective of whether it actually was real.
When activity in the fusiform gyrus was strong, people were more likely to indicate that the pattern was really there.
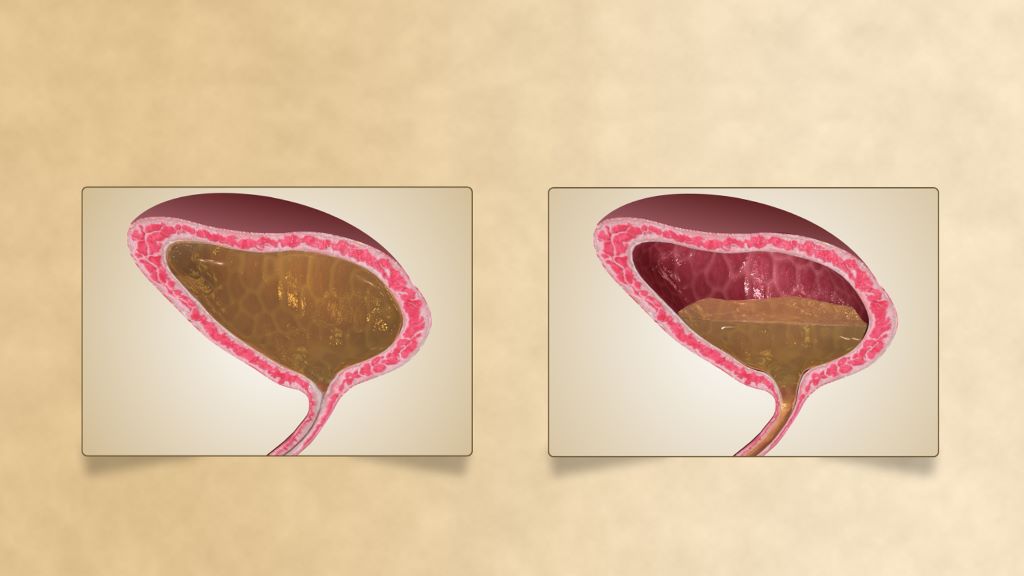
Usually, activation in the fusiform gyrus is weaker during imagination than during perception, which helps the brain keep the two apart. However, this study showed that sometimes when participants imagined very vividly, activation of the fusiform gyrus was very strong and participants confused their imagination for reality.
Senior author, Professor Steve Fleming (UCL Psychology & Language Sciences) said: “The brain activity in this area of visual cortex matched the predictions from a computer simulation on how the difference between internally and externally generated experience is determined.”
Dr Dijkstra added: “Our findings suggest that the brain uses the strength of sensory signals to distinguish between imagination and reality.”
The study also showed that the fusiform gyrus collaborates with other brain areas to help us decide what is real and what is imagined.
Specifically, activity in the anterior insula – a brain region in the prefrontal cortex (the front part of the brain that acts as a control centre for tasks such as decision making, problem solving and planning) – increased in line with activity in the fusiform gyrus when participants said something was real, even if it was in fact imagined.
Professor Fleming said: “These areas of the prefrontal cortex have previously been implicated in metacognition – the ability to think about our own minds. Our results indicate that the same brain areas are also involved in deciding what is real.”
These results offer new insights into what might go wrong in the brain during psychiatric conditions like schizophrenia where patients struggle keeping apart imagination and reality. The findings may also inform future virtual reality technologies by identifying how and when imagined experiences feel real.
Source: University College London