MIT Engineers Turn Skin Cells Directly into Neurons for Cell Therapy
A new, highly efficient process for performing this conversion could make it easier to develop therapies for spinal cord injuries or diseases like ALS.
Anne Trafton | MIT News
Converting one type of cell to another – for example, a skin cell to a neuron – can be done through a process that requires the skin cell to be induced into a “pluripotent” stem cell, then differentiated into a neuron. Researchers at MIT have now devised a simplified process that bypasses the stem cell stage, converting a skin cell directly into a neuron.
Working with mouse cells, the researchers developed a conversion method that is highly efficient and can produce more than 10 neurons from a single skin cell. If replicated in human cells, this approach could enable the generation of large quantities of motor neurons, which could potentially be used to treat patients with spinal cord injuries or diseases that impair mobility.
“We were able to get to yields where we could ask questions about whether these cells can be viable candidates for the cell replacement therapies, which we hope they could be. That’s where these types of reprogramming technologies can take us,” says Katie Galloway, the W. M. Keck Career Development Professor in Biomedical Engineering and Chemical Engineering.
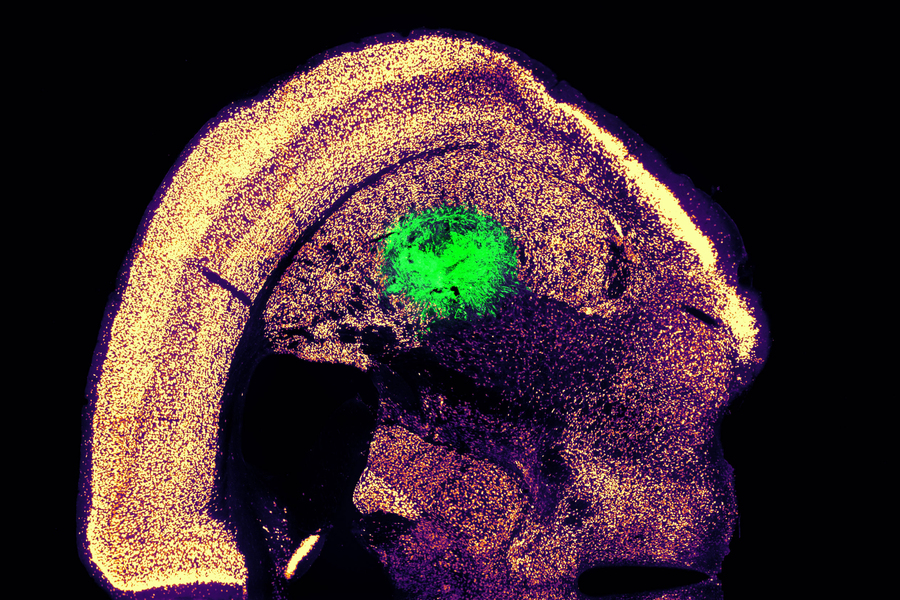
As a first step toward developing these cells as a therapy, the researchers showed that they could generate motor neurons and engraft them into the brains of mice, where they integrated with host tissue.
Galloway is the senior author of two papers describing the new method, which appear today in Cell Systems. MIT graduate student Nathan Wang is the lead author of both papers.
From skin to neurons
Nearly 20 years ago, scientists in Japan showed that by delivering four transcription factors to skin cells, they could coax them to become induced pluripotent stem cells (iPSCs). Similar to embryonic stem cells, iPSCs can be differentiated into many other cell types. This technique works well, but it takes several weeks, and many of the cells don’t end up fully transitioning to mature cell types.
“Oftentimes, one of the challenges in reprogramming is that cells can get stuck in intermediate states,” Galloway says. “So, we’re using direct conversion, where instead of going through an iPSC intermediate, we’re going directly from a somatic cell to a motor neuron.”
Galloway’s research group and others have demonstrated this type of direct conversion before, but with very low yields – fewer than 1 percent. In Galloway’s previous work, she used a combination of six transcription factors plus two other proteins that stimulate cell proliferation. Each of those eight genes was delivered using a separate viral vector, making it difficult to ensure that each was expressed at the correct level in each cell.
In the first of the new Cell Systems papers, Galloway and her students reported a way to streamline the process so that skin cells can be converted to motor neurons using just three transcription factors, plus the two genes that drive cells into a highly proliferative state.
Using mouse cells, the researchers started with the original six transcription factors and experimented with dropping them out, one at a time, until they reached a combination of three – NGN2, ISL1, and LHX3 — that could successfully complete the conversion to neurons.
Once the number of genes was down to three, the researchers could use a single modified virus to deliver all three of them, allowing them to ensure that each cell expresses each gene at the correct levels.
Using a separate virus, the researchers also delivered genes encoding p53DD and a mutated version of HRAS. These genes drive the skin cells to divide many times before they start converting to neurons, allowing for a much higher yield of neurons, about 1100 percent.
“If you were to express the transcription factors at really high levels in nonproliferative cells, the reprogramming rates would be really low, but hyperproliferative cells are more receptive. It’s like they’ve been potentiated for conversion, and then they become much more receptive to the levels of the transcription factors,” Galloway says.
The researchers also developed a slightly different combination of transcription factors that allowed them to perform the same direct conversion using human cells, but with a lower efficiency rate – between 10 and 30 percent, the researchers estimate. This process takes about five weeks, which is slightly faster than converting the cells to iPSCs first and then turning them into neurons.
Implanting cells
Once the researchers identified the optimal combination of genes to deliver, they began working on the best ways to deliver them, which was the focus of the second Cell Systems paper.
They tried out three different delivery viruses and found that a retrovirus achieved the most efficient rate of conversion. Reducing the density of cells grown in the dish also helped to improve the overall yield of motor neurons. This optimised process, which takes about two weeks in mouse cells, achieved a yield of more than 1000 percent.
Working with colleagues at Boston University, the researchers then tested whether these motor neurons could be successfully engrafted into mice. They delivered the cells to a part of the brain known as the striatum, which is involved in motor control and other functions.
After two weeks, the researchers found that many of the neurons had survived and seemed to be forming connections with other brain cells. When grown in a dish, these cells showed measurable electrical activity and calcium signaling, suggesting the ability to communicate with other neurons. The researchers now hope to explore the possibility of implanting these neurons into the spinal cord.
The MIT team also hopes to increase the efficiency of this process for human cell conversion, which could allow for the generation of large quantities of neurons that could be used to treat spinal cord injuries or diseases that affect motor control, such as ALS. Clinical trials using neurons derived from iPSCs to treat ALS are now underway, but expanding the number of cells available for such treatments could make it easier to test and develop them for more widespread use in humans, Galloway says.
The research was funded by the National Institute of General Medical Sciences and the National Science Foundation Graduate Research Fellowship Program.
Reprinted with permission of MIT News






