Breast Cancer Treatment Linked to a Reduction in Alzheimer’s Disease Risk

A Korean population-based cohort study investigated the risk of Alzheimer’s disease (AD) among breast cancer survivors compared to age-matched controls without cancer. The study, published in JAMA Network Open, found that breast cancer survivors had an 8% lower risk of AD than controls, with a significant association in survivors over 65 years old – though the effect did not persist past five years. Radiotherapy was associated with a lower risk of AD among breast cancer survivors – but not other treatments.
Breast cancer survivors may experience long-term health consequences, including cognitive function and risk of dementia. The risk of AD among breast cancer survivors is still unclear and may vary depending on age at diagnosis, treatment received, and time since treatment.
Previous studies reported mixed results on the risk of AD among breast cancer survivors, with some finding no increase in risk and others finding a 35% increased risk for those diagnosed at age 65 or older. These studies have been hampered by a number of methodological issues, including not accounting for risk factors.
Cytotoxic chemotherapy can cause cognitive decline termed ‘chemobrain’. Other chemotherapy drugs such as anthracycline may reduced AD risk by reducing the formation of amyloid deposits. Endocrine therapy may increase the risk of dementia by lowering oestrogen, but studies suggest that the use of tamoxifen and aromatase inhibitors is associated with a lower risk of AD. An increase in dementia is seen in radiotherapy for head and neck cancers.
To investigate the risk of AD among breast cancer survivors, researchers used the Korean National Health Insurance Service (K-NHIS) database, exploring whether there is an association with cancer treatment and various confounding factors.
Among 70 701 breast cancer survivors (mean age, 53.1 years), 1229 cases of AD were detected, with an incidence rate of 2.45 per 1000 person-years. Survivors exhibited a slightly lower risk of AD compared with cancer-free controls, especially among individuals 65 years or older (SHR, 0.92; 95% CI, 0.85-0.99). But landmark analyses found that this lower risk did not persist beyond five years of survival. Radiotherapy was associated with reduced risk of AD among survivors, while chemotherapy and endocrine therapy had no significant impact. Anthracycline use, however, did show a non-significant decrease in risk.
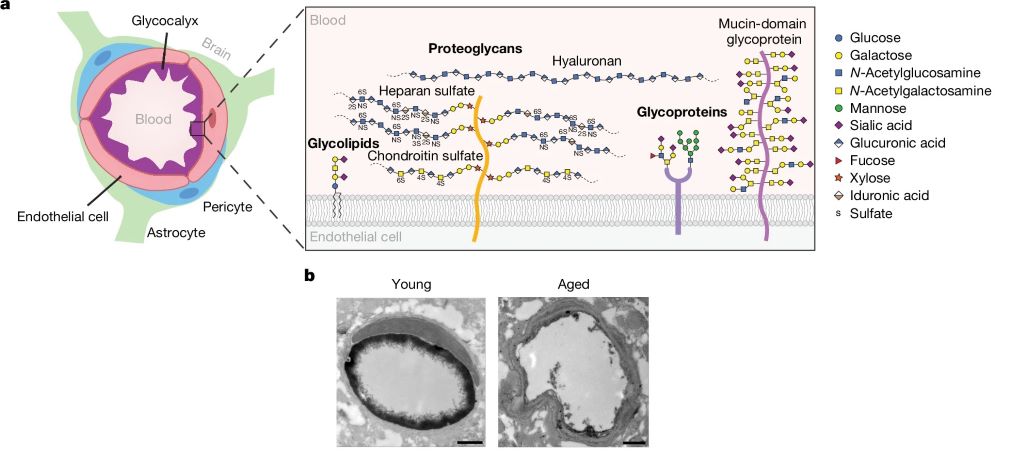
Differences in doses and timing of radiotherapy may influence the effects. The incident exposure to the brain is estimated to be 0.2Gy from a breast cancer radiotherapy dose of 50Gy. A pilot study found that patients with AD who received low-dose whole-brain radiotherapy at 3Gy showed a temporary improvement in cognitive function. This improvement is believed to be due to a neuroprotective effect on microglia. Other studies have noted a transient risk reduction for AD in breast cancer radiotherapy; however, patients receiving radiotherapy usually do so in conjunction with breast-conserving surgery – those opting for this procedure are younger, with fewer comorbidities and smaller tumours.
The study suggests that cancer treatment may have benefits against AD development, but the risk of AD may differ depending on the duration of survival.
The findings indicate that breast cancer treatment may not directly lead to AD, and that managing modifiable risk factors for AD, such as smoking and diabetes, is a feasible option to lower AD risk among breast cancer survivors.