Tirzepatide Found to Protect against Worsening Heart Failure
The diabetes drug tirzepatide can reduce the risk of death or worsening heart failure for patients with heart failure, preserved heart pump function and obesity, new research from UVA Health reveals.
Researchers tested the GLP-1 receptor agonist in the SUMMIT clinical trial, where a total of 731 patients with diastolic heart failure and a body mass index (BMI) of 30 or above were randomised to receive injections of either tirzepatide or a harmless placebo. The researchers then followed the patients for a median period of two years. Tirzepatide is also prescribed as a weight loss drug in certain countries.
During that time, 56 placebo recipients died or suffered worsening heart failure, compared with only 36 of those receiving tirzepatide. Participants taking tirzepatide also lost 11.6% of their body weight.
“This class of drugs continue to show benefits far beyond weight loss,” said researcher Christopher Kramer, MD, chief of UVA Health’s Division of Cardiovascular Medicine. “This drug will become an important part of the armamentarium for patients with obesity-related heart failure and preserved heart function.”
Obesity and heart failure
Obesity is a major contributing factor to heart failure, so Kramer and his collaborators in the SUMMIT trial wanted to see if tirzepatide, a weight-loss drug already approved by the federal Food and Drug Administration, could help.
The trial found that tirzepatide offered substantial benefits for managing diastolic heart failure, reducing deaths, preventing hospitalizations and generally benefiting recipients’ health and quality of life. For example, recipients saw improvements in how far they could walk in six minutes, as well as substantial decreases in a biological indictor used to measure inflammation and predict risk of serious cardiovascular events.
Side effects seen in the tirzepatide group consisted of gastrointestinal issues such as nausea and diarrhea, and these were mostly mild or moderate, the researchers reported Saturday at a meeting of the American Heart Association in Chicago.
Tirzepatide Findings
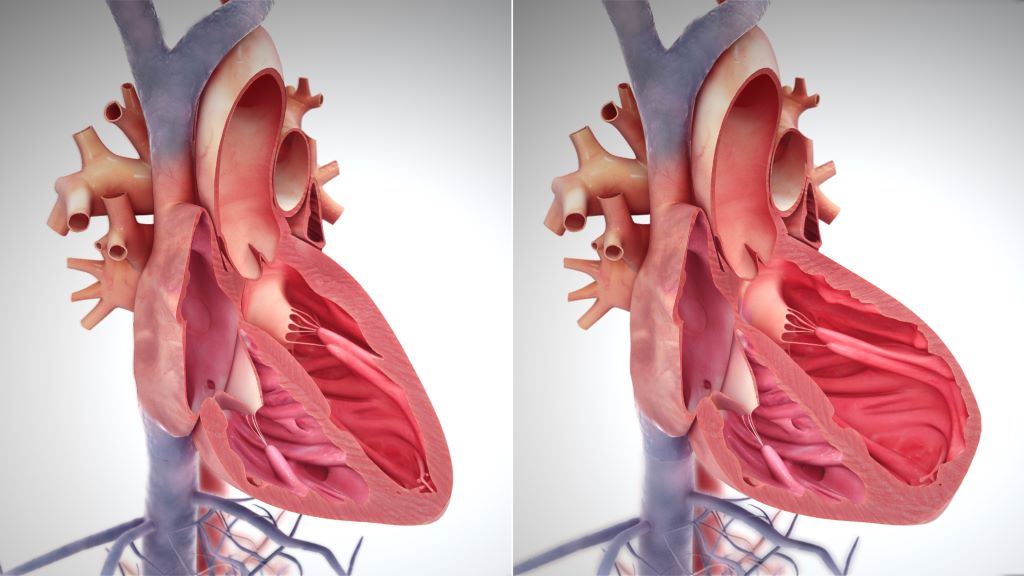
Kramer, a cardiovascular imager, also led a magnetic resonance imaging substudy looking at how tirzepatide affected recipients’ heart structure and function. The researchers found beneficial reductions in both left ventricular mass (weight of the heart) and in the amount of surrounding fat tissue. The reduction in LV mass correlated with the reduction in body weight, as well as with decreases in left ventricular volumes.
“This drug is reversing the abnormal properties of the heart brought on by obesity,” Kramer said. “There is much more to these drugs than weight loss alone.”
The findings from these studies by Kramer and his fellow researchers from SUMMIT are being published simultaneous with the American Heart meeting in Chicago in four separate manuscripts, including the New England Journal of Medicine, Nature Medicine, Circulation and the Journal of the American College of Cardiology.






