Clinical Trial Shows a Constipation Drug Aids Kidney Function

Chronic kidney disease (CKD) is a major health issue worldwide. Many patients end up requiring regular dialysis to avoid kidney failure and stay alive. Despite the severity of the condition, there are currently no drugs available that improve kidney function. A research group led by Tohoku University Graduate School of Medicine’s Professor Takaaki Abe has found a remarkable solution to treat patients with CKD by co-opting a drug typically used for constipation. This is the first time that this drug (lubiprostone) was shown to prevent the decline of renal function in patients with CKD.
“We noticed that constipation is a symptom that often accompanies CKD, and decided to investigate this link further,” explains Abe. “Essentially, constipation disrupts the intestinal microbiota, which worsens kidney function. Working backwards, we hypothesised that we could improve kidney function by treating constipation.”
To address this issue, the group conducted a multicentre Phase II clinical trial (LUBI-CKD TRIAL) at nine Japanese medical institutions, enrolling 150 patients with moderate CKD. This study evaluated the effects of lubiprostone on kidney function. The results showed that, compared to the placebo group, the decline in kidney function (defined as the estimated glomerular filtration rate: eGFR) was suppressed in a dose-dependent manner in patients treated with 8µg or 16µg of lubiprostone.
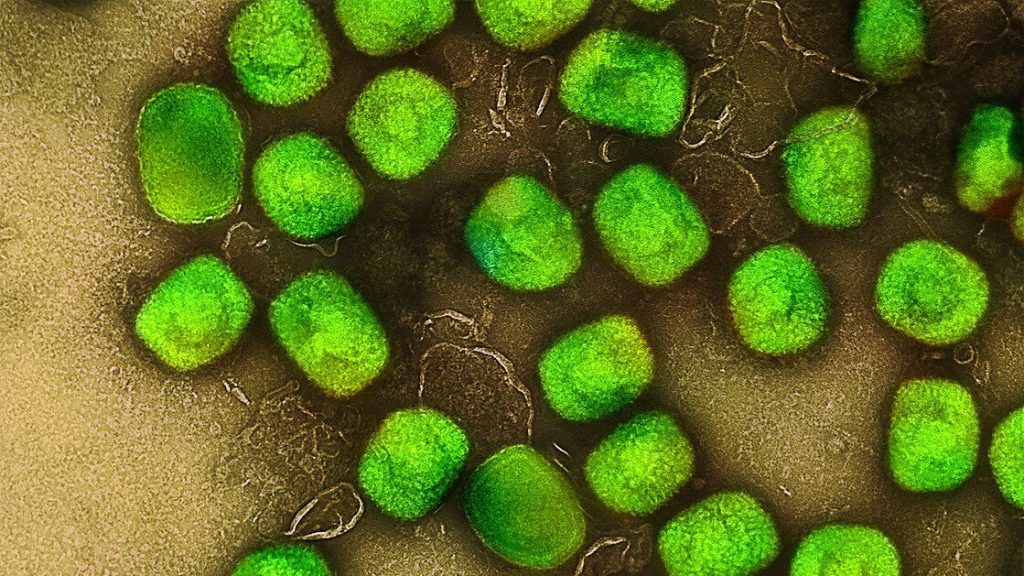
The researchers also investigated the mechanism underlying how this effect occurred. They found that lubiprostone increases spermidine production, which improves mitochondrial function by promoting bacterial growth in the gut. The improved mitochondrial function was seen to exert a renoprotective effect – suppressing further kidney damage.
Going forward, the research team has plans to validate the trial results in a larger population (Phase 3 clinical trial) and advance the exploration of biomarkers that predict treatment efficacy. Their goal is to provide each patient with CKD the optimal treatment plan tailored to their needs. This discovery has the potential to significantly transform the conventional approach to CKD treatment, which primarily focuses on reducing uremic toxins.
These findings suggest a new therapeutic strategy in which laxatives suppress renal function decline. This strategy is expected to contribute to the development of treatments for not only CKD, but also mitochondrial dysfunction disorders. The results of this study were published in Science Advances on August 30, 2025.
Source: Tohoku University