Scientists Solve Epstein-Barr Virus Mystery

Medical science has not yet been able to explain why the Epstein-Barr virus triggers infectious mononucleosis (IM) in some people with initial infections and not in others. But now researchers have identified a unusual T cell response to the virus as the cause, and as a potential target for the development of vaccines. The findings were recently published in the journal Blood.
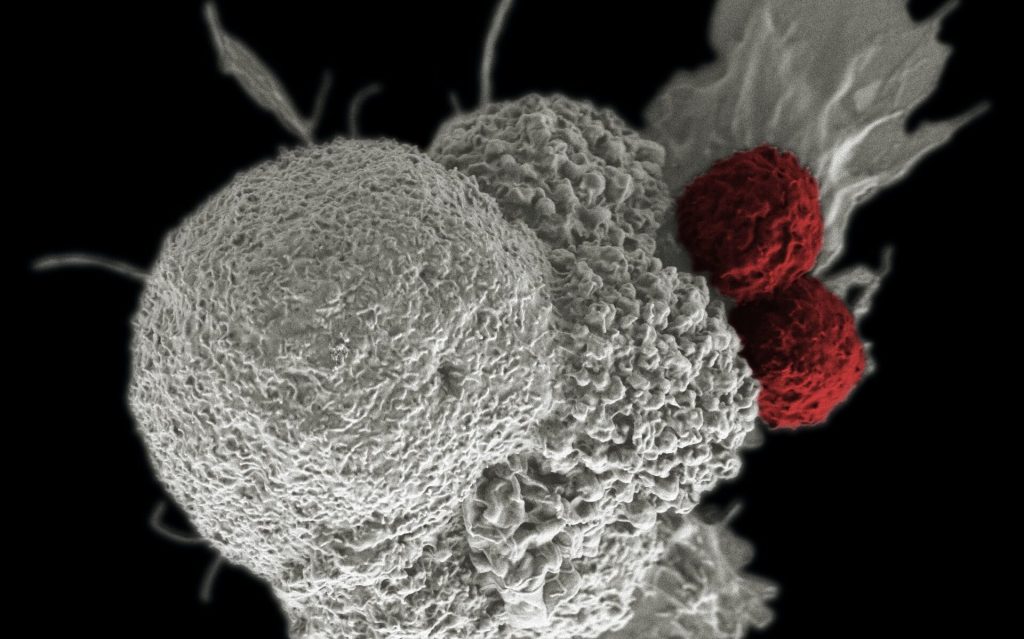
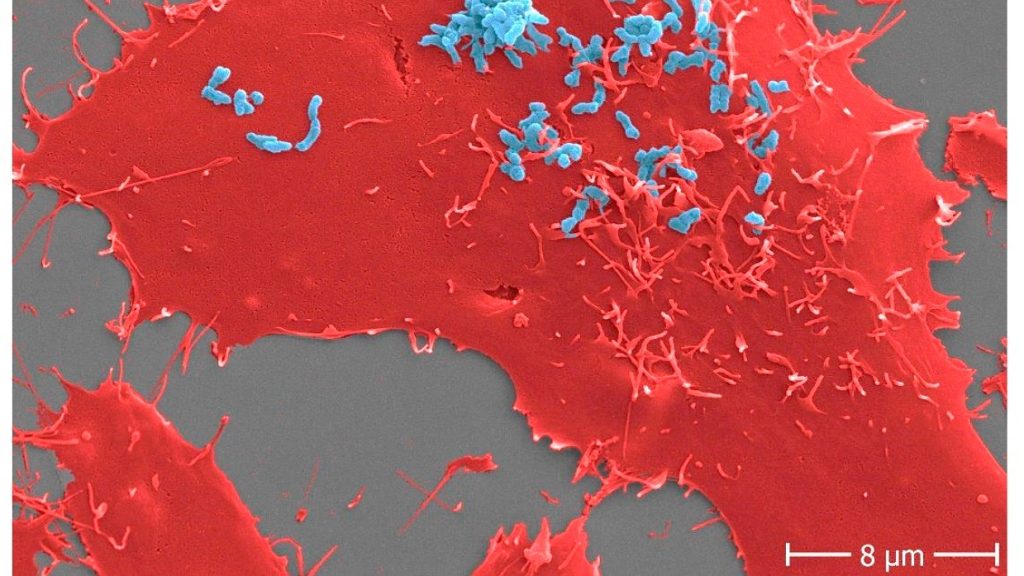
T cells normally fight the proliferation of the Epstein-Barr virus (EBV) in humans as part of an antiviral immune response. In this response, certain EBV components (peptides) are presented to the T cells by a specific molecule (HLA-E), which is found on the surface of cells infected with EBV. This triggers a non-classical T-cell response that leads to the destruction of the infected cells. Due to a genetic variation (HLA-E*0103/0103), about one third of the population naturally has more HLA-E molecules on EBV-infected cells.
A recently published study has shown that the risk of developing IM following first-time infection with the Epstein-Barr virus depends strongly on this EBV-specific immune response.
“Our research revealed that people with the HLA-E*0103/0103 genetic variation have a lower risk of developing infectious mononucleosis than those who do not have the variation. Our experiments in the lab showed that this gene variation is associated with a highly pronounced EBV-specific -non-classical — immune response,” explained Hannes Vietzen from MedUni Vienna’s Center for Virology, the first author of the study.
Preventive and diagnostic possibilities
EBV is one of the most common viral infections in humans. On initial infection, the virus causes IM in some children and young adults; this disease is characterised by non-specific symptoms, such as fever, as well as exhaustion that in some cases can last for several months. Until now, it was unclear why a first-time EBV infection only leads to IM in a minority of people, while most do not present any symptoms whatsoever. The immune response that the researchers identified could also be a target for research into preventive measures: “This immune response was still measurable years after the initial EBV infection and generally provides long-lasting protection against reinfection with Epstein-Barr, so it might be worth focusing our attention on this mechanism with a view to developing new vaccines in future,” said Hannes Vietzen, looking ahead.
Another finding from the study could also open up new diagnostic options: “The combination of the unfavourable HLA-E genetic variation with certain EBV peptides also appears to play an important role in the development of EBV-associated lymphomas in transplant recipients,” Hannes Vietzen commented. “Analysis of the EBV strains found in these patients could be helpful in identifying high-risk patients at an early stage and treating them in good time.”
Source: Medical University of Vienna