Gluten Free Diet Reduces Coeliac Symptoms – and ‘Good’ Gut Bacteria

A research team led by the University of Nottingham has used magnetic resonance imaging (MRI) to better understand the impact a gluten free diet has on people with coeliac disease, which could be the first step towards finding new ways of treating the condition.
The MARCO study – MAgnetic Resonance Imaging in COliac disease is published in Clinical Gastroenterology and Hepatology (CGH) (link connects to BioRxiv copy).
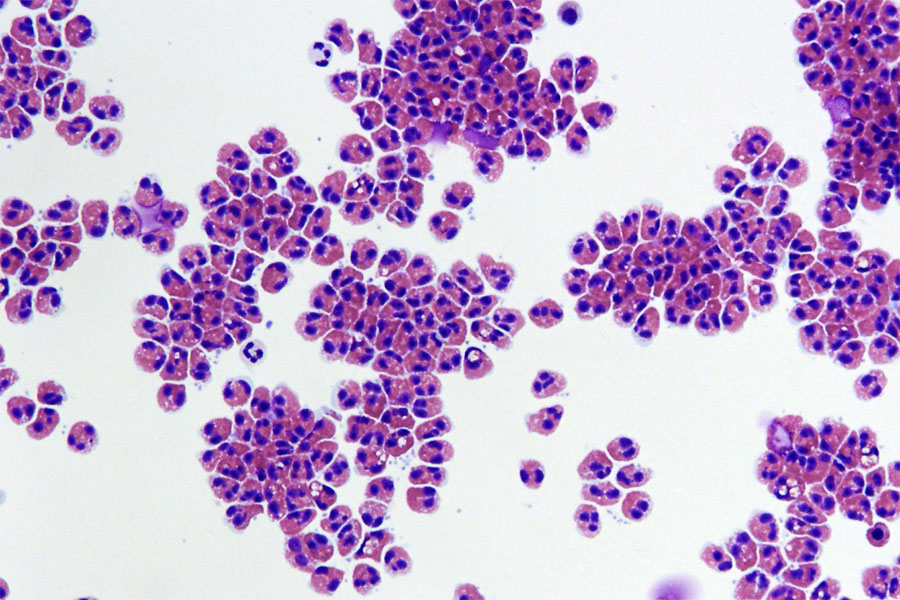
Coeliac disease is a chronic condition affecting around one person in every 100 in the general population. When people with coeliac disease eat gluten, which is found in pasta and bread, their immune system produces an abnormal reaction that inflames and damages the gut tissue and causes symptoms such as abdominal pain and bloating.
The only treatment is a life- long commitment to a gluten free diet, which helps recovery of the gut tissue but still leaves many patients with gastrointestinal symptoms.
Luca Marciani, Professor of Gastrointestinal Imaging at the University, led the study. He said: “Despite being a common chronic condition, we still don’t precisely know how coeliac disease affects the basic physiological functioning of the gut and how the gluten free diet treatment may further change this.
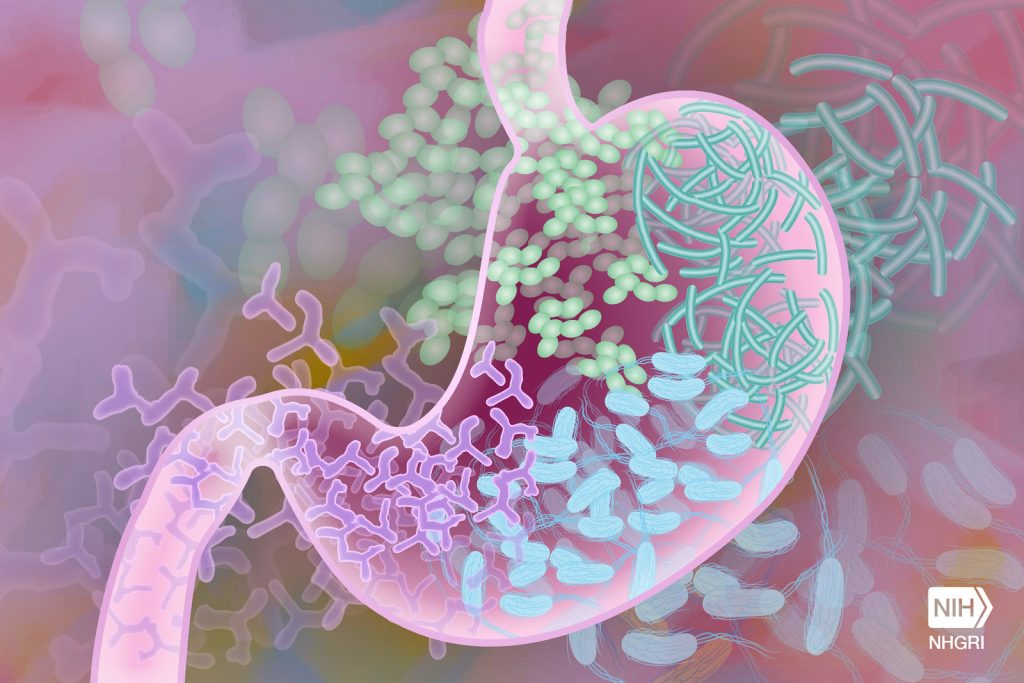
“We launched the MARCO study to try and address this issue, by using MRI along with gut microbiome analysis to give us new insights into how a gluten-free diet affects people with coeliac disease.”
The team recruited 36 people who had just been diagnosed with coeliac disease and 36 healthy volunteers to participate in the study. Images were taken of their guts with MRI, along with blood and stool samples. The patients then followed a gluten free diet for one year and came back to repeat the study. The healthy participants came back one year later too and repeated the study, but they did not follow any diet treatment.
The study found that the newly diagnosed patients with coeliac disease had more gut symptoms, more fluid in the small bowel and that the transit of food in the bowel was slower than in the healthy controls.
The microbiota (the ‘bugs’ living in the colon) of the patients showed higher levels of ‘bad bugs’ such as E.coli. After one year of a gluten free diet, gut symptoms, bowel water and gut transit improved in the patients, but without returning to normal values. But the gluten free diet also reduced some of the ‘good bugs’ in the microbiota, such as Bifidobacteria associated with reduced intake of starch and wheat nutrients, due to the different diet.
The patient study was conducted by Radiographer Dr Carolyn Costigan, from Nottingham University Hospitals, as part of her PhD studies at the University of Nottingham.
It was particularly interesting to see how the imaging results on gut function correlated with changes in the ‘bugs’ in the colon microbiota. The findings increase our understanding of gut function and physiology in coeliac disease and open the possibility of developing prebiotic treatments to reverse the negative impact of the gluten free diet on the microbiome.”
Luca Marciani, Professor of Gastrointestinal Imaging
Dr Frederick Warren from the Quadram Institute, which contributed to the research, said: “This study is the result of an exciting and innovative research collaboration bringing together medical imaging technology and gut microbiome analysis. We provide important insights which pave the way for future studies which may identify novel approaches to alleviate long-term symptoms in coeliac patients.”
Source: University of Nottingham