Existing Drug Class May Help Patients with Immunotherapy-resistant Melanoma
Increased activity in a specific biological pathway may explain why many patients with a deadly form of skin cancer do not respond to the latest cancer treatments, a new study shows.
Publishing in the journal Cancer Research, the study featured data generated from experiments with human tissues and cells from patients with advanced melanoma that were implanted into mice. Results uncovered therapeutic targets that could limit melanoma growth in patients whose cancer failed to respond to initial treatment with immune checkpoint inhibitors.
Led by researchers at NYU Langone Health and its Perlmutter Cancer Center, the study focused on a subgroup of melanoma patients with mutations in the neurofibromin 1 (NF1) gene. NF1 mutations are just one type among several mutations, including those in the BRAF, NRAS, and PARP genes, that are linked to many cases of cancer, particularly melanoma. As many as 27% of melanoma patients are estimated to have NF1 mutations.
While immunotherapy, which stimulates the immune system to attack cancer cells as it would an invading virus, has proved to be a successful treatment, it does not work well for more than half of NF1-mutant melanoma patients.
“There is a pressing need for new drug therapies for melanoma patients with neurofibromin 1 mutations that do not respond to the latest immunotherapy, and for which there are no subsequent effective treatment options,” said study lead investigator Milad Ibrahim, PhD. Ibrahim is a postdoctoral fellow in the Dr Iman Osman Laboratory in the Ronald O. Perelman Department of Dermatology at the NYU Grossman School of Medicine.
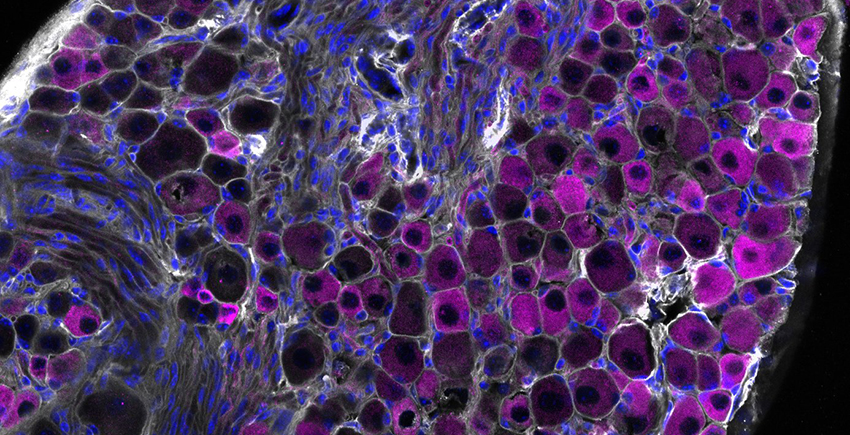
To investigate why these patients were treatment resistant, investigators examined tumour cells from 30 melanoma patients who did not respond to immunotherapy. NF1 mutations were found in 40% of these melanoma samples. The samples came from NYU Langone’s extensive repository from more than 6000 melanoma patients.
Molecular testing showed that the signalling pathway built around a protein called epidermal growth factor receptor (EGFR) was more active in NF1 mutant melanoma cells than in cells with other melanoma-gene mutations. Increased EGFR activity has long been linked to abnormal cell growth in tumours and shorter survival with various cancers. The researchers also found that NF1 mutant melanoma cells depended on increased EGFR activity for survival, regardless of the presence of other mutations.
Because EGFR-inhibiting drugs are already used to treat some head and neck cancers, as well as colorectal and lung cancers, researchers then tested two drugs in the class, cetuximab and afatinib, in both NF1 mutant cell cultures and cancer cell lines without NF1 mutations. After transplanting both tumour cell types into mice and treating them with these drugs, results showed that both EGFR inhibitors were effective against cells and transplanted tumours with NF1 mutations, and they had no effect on melanomas without NF1 mutations.
“Our study results reveal a unique vulnerability in melanoma patients with neurofibromin 1 mutations, that an overexpression of the epidermal growth factor receptor pathway is essential for their survival and growth,” said the study’s senior investigator, Professor Iman Osman, MD.
“While further tests are needed, our results support a novel approach of deploying EGFR inhibitors either alone or in combination with other immunotherapies for treatment of melanoma patients whose tumours harbour NF1 mutation,” said the study’s co-senior investigator, Associate Professor Markus Schober, PhD.
However, Schober says this requires further testing in a clinical trial, which the research team plans to develop. He adds that if trial findings prove successful, the team’s research could provide a lifeline for many of these melanoma patients.
Source: NYU Langone Health