Paxlovid may Interact with Common Heart Drugs

Nirmatrelvir-ritonavir (Paxlovid) is often given to heart disease patients with symptomatic COVID to prevent progression to severe disease – but it can interact with some previously prescribed medications. A review paper published in the Journal of the American College of Cardiology examines the potential drug-drug interactions (DDIs) between Paxlovid and commonly used cardiovascular medications, as well as potential options to mitigate severe adverse effects.
“Awareness of the presence of drug-drug interactions of Paxlovid with common cardiovascular drugs is key. System-level interventions by integrating drug-drug interactions into electronic medical records could help avoid related adverse events,” said Sarju Ganatra, MD, senior author of the review.
He continued: “The prescription of Paxlovid could be incorporated into an order set, which allows physicians, whether it be primary care physicians or cardiology providers, to consciously rule out any contraindications to the co-administration of Paxlovid. Consultation with other members of the health care team, particularly pharmacists, can prove to be extremely valuable. However, a health care provider’s fundamental understanding of the drug-drug interactions with cardiovascular medications is key.”
In December 2021, Paxlovid received emergency use authorisation from the US Food and Drug Administration as an oral antiviral agent for the treatment of symptomatic, non-hospitalised adults with mild to moderate COVID infection who are at high risk for progression to severe disease. Patients with heart disease and other risk factors, including diabetes, high blood pressure, chronic kidney disease and smoking make up a large portion of the high-risk population for whom Paxlovid is beneficial.
According to the authors, Paxlovid has been shown to be very effective in patients with existing heart disease, but it has significant DDIs with commonly used cardiovascular medications, highlighting the importance for all clinicians to be familiar with these DDIs. As there is limited clinical information regarding DDI-related adverse events, the authors used existing knowledge and data regarding how therapies like Paxlovid typically react with other medications to provide guidance regarding potential interactions and the associated likely consequences based on the degree of interaction.
The review provides an in-depth overview of a variety of cardiovascular medications used to treat many forms of heart disease. Five of the most important cardiovascular drug interactions with Paxlovid to be aware of include:
- Anti-arrhythmic agents
- Many anti-arrhythmic agents are metabolised in a way that increases plasma levels when co-administered with Paxlovid. While it may be possible to start Paxlovid after 2–2.5-day temporary discontinuation of the anti-arrhythmic agents, this may not be feasible from a practical standpoint. Clinicians are advised to consider alternative COVID therapies and avoid co-administration of these agents with Paxlovid. Sotalol, another anti-arrhythmic agent, is renally cleared and does not interact with Paxlovid.
- Antiplatelet agents and anticoagulants
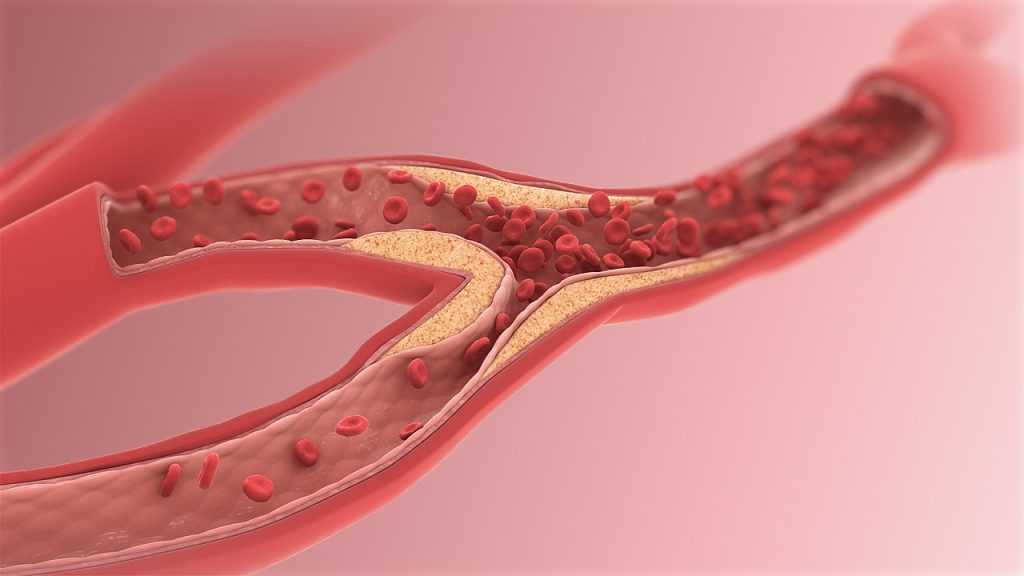
- Antiplatelet agents are used for the treatment of coronary artery disease, particularly if a patient has received a stent. Aspirin and prasugrel are safe to co-administer with Paxlovid. There is an increased risk of blood clots when Paxlovid is given alongside clopidogrel and an increased risk of bleeding when given with ticagrelor. When possible, these agents should be switched to prasugrel. If patients have contraindication to taking prasugrel, then co-administration of Paxlovid should be avoided and alternative COVID therapies should be considered.
- Anticoagulants such as warfarin may be co-administered with Paxlovid but require close monitoring of clotting factors in bloodwork. The plasma levels of all direct oral anticoagulants increase when co-administered with Paxlovid, therefore dose adjustment or temporary discontinuation and use of alternative anticoagulants may be required.
- Certain statins
- Co-administration of simvastatin or lovastatin with Paxlovid can lead to increased plasma levels and subsequent myopathy and rhabdomyolysis, a condition in which the breakdown of muscle tissue releases a damaging protein into the bloodstream. These agents should be stopped prior to initiation of Paxlovid. A dose reduction of atorvastatin and rosuvastatin is reasonable when co-administered with Paxlovid. The other statins are considered safe when given along with Paxlovid.
- Ranolazine
- Plasma concentration of ranolazine, used to treat angina and other heart-related chest pain, is exponentially increased in the presence of CPY450 inhibitors like Paxlovid, thereby increasing the risk of clinically significant QT prolongation and torsade de pointes (a type of arrhythmia). Co-administration of Paxlovid is therefore contraindicated. Temporary discontinuation of ranolazine is advised if prescribing Paxlovid.
- Immunosuppressive agents
- The plasma levels of immunosuppressive agents prescribed for patients who have undergone heart transplantation exponentially rise to toxic levels when co-administered with Paxlovid. Temporary reduction of dosing of immunosuppressive agents would require frequent monitoring and be logistically difficult. Therefore, alternative COVID therapies should be considered in these patients.
The authors conclude awareness and availability of other COVID therapies enable clinicians to offer alternative treatment options to patients who are unable to take Paxlovid due to DDIs.