Amid Surge in Cases, UK’s NHS to Offer Gonorrhoea Vaccine
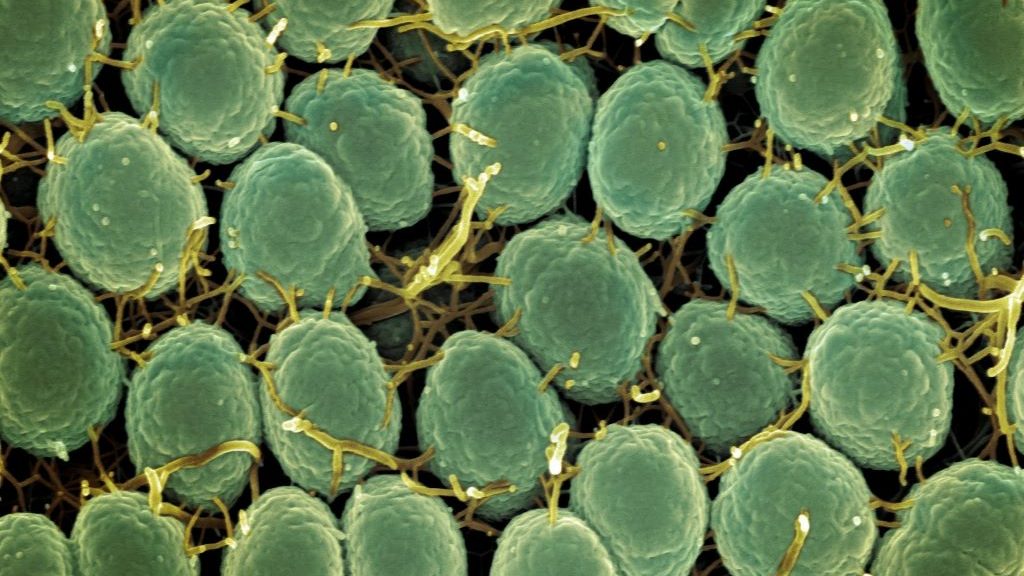
Neisseria gonorrhoeae Bacteria Scanning electron micrograph of Neisseria gonorrhoeae bacteria, which causes gonorrhoea. Captured by the Research Technologies Branch (RTB) at the NIAID Rocky Mountain Laboratories (RML) in Hamilton, Montana. Credit: NIAID. Photo by National Institute of Allergy and Infectious Diseases on Unsplash
In the midst of a record high in gonorrhoea cases, the NHS is to offer a gonorrhoea vaccine to gay and bisexual men with a history of multiple partners or a sexually transmitted infection (STI), the BBC reports. The gonorrhoea vaccination, which is actually a repurposed meningococcal vaccine, is estimated only to be 30–40% effective. Research shows, however, that this will be sufficient to reduce cases and their attendant costs to the NHS.
Gonorrhoea is caused by the bacterium Neisseria gonorrhoeae and is typically transmitted by having intercourse without a condom. It can cause pain, unusual discharge, genital inflammation and infertility. Evidence has shown that the MeNZB and four-component serogroup B meningococcal (4CMenB) vaccines, designed against Neisseria meningitidis, can also offer protection against gonorrhoea.
In 2023, there were more than 85 000 cases – the highest since records began in 1918. A study published in The Lancet estimates that gonorrhoea vaccination would prevent 100 000 cases, saving the NHS £7.9 million over the next decade.
While gonorrhoea is treatable with antibiotics, resistance is growing and there is concern that it may eventually become untreatable. According to The Guardian, some cases are now “extensively drug resistant” (XDR) – not responsive to ceftriaxone or the second line of treatment. There were 17 cases of ceftriaxone-resistant gonorrhoea between January 2024 and March 2025, the UK Health Security Agency (UKHSA) reported.
Over the same period, nine XDR cases were reported, while between 2022 and 2023, there were only five.
The people most affected by gonorrhoea in the UK are the 16 to 25 age group, gay and bisexual men, and those of black and Caribbean ancestry. The study’s scenario for vaccinating at-risk populations included those who had more than five sexual partners per year or who had a positive gonorrhoea test.
The vaccine, costing about £8 per dose, is cost-effective when administered to this at-risk group of men, rather than adolescents. Despite this, clinicians will be able to offer the vaccine to anyone who, in their judgment, would benefit from it. Other vaccines such as for mpox – another STI with high transmission between gay and bisexual men – and hepatitis will also be offered.


