How ‘Brain Cleaning’ While We Sleep May Lower Our Risk of Dementia

Julia Chapman, Macquarie University; Camilla Hoyos, Macquarie University, and Craig Phillips, Macquarie University
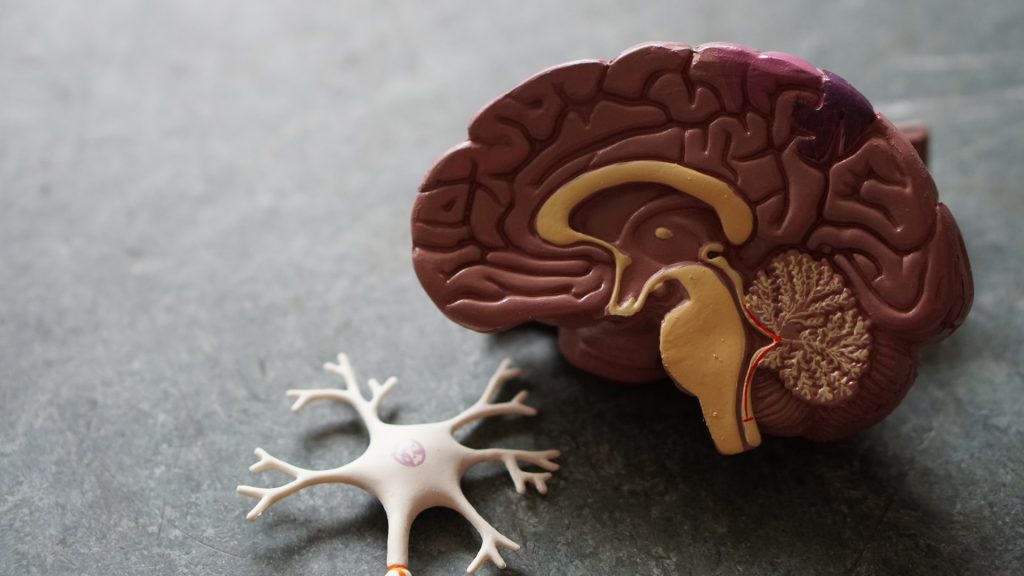
The brain has its own waste disposal system – known as the glymphatic system – that’s thought to be more active when we sleep.
But disrupted sleep might hinder this waste disposal system and slow the clearance of waste products or toxins from the brain. And researchers are proposing a build-up of these toxins due to lost sleep could increase someone’s risk of dementia.
There is still some debate about how this glymphatic system works in humans, with most research so far in mice.
But it raises the possibility that better sleep might boost clearance of these toxins from the human brain and so reduce the risk of dementia.
Here’s what we know so far about this emerging area of research.
Why waste matters
All cells in the body create waste. Outside the brain, the lymphatic system carries this waste from the spaces between cells to the blood via a network of lymphatic vessels.
But the brain has no lymphatic vessels. And until about 12 years ago, how the brain clears its waste was a mystery. That’s when scientists discovered the “glymphatic system” and described how it “flushes out” brain toxins.
Let’s start with cerebrospinal fluid, the fluid that surrounds the brain and spinal cord. This fluid flows in the areas surrounding the brain’s blood vessels. It then enters the spaces between the brain cells, collecting waste, then carries it out of the brain via large draining veins.
Scientists then showed in mice that this glymphatic system was most active – with increased flushing of waste products – during sleep.
One such waste product is amyloid beta (Aβ) protein. Aβ that accumulates in the brain can form clumps called plaques. These, along with tangles of tau protein found in neurons (brain cells), are a hallmark of Alzheimer’s disease, the most common type of dementia.
In humans and mice, studies have shown that levels of Aβ detected in the cerebrospinal fluid increase when awake and then rapidly fall during sleep.
But more recently, another study (in mice) showed pretty much the opposite – suggesting the glymphatic system is more active in the daytime. Researchers are debating what might explain the findings.
So we still have some way to go before we can say exactly how the glymphatic system works – in mice or humans – to clear the brain of toxins that might otherwise increase the risk of dementia.
Does this happen in humans too?
We know sleeping well is good for us, particularly our brain health. We are all aware of the short-term effects of sleep deprivation on our brain’s ability to function, and we know sleep helps improve memory.
In one experiment, a single night of complete sleep deprivation in healthy adults increased the amount of Aβ in the hippocampus, an area of the brain implicated in Alzheimer’s disease. This suggests sleep can influence the clearance of Aβ from the human brain, supporting the idea that the human glymphatic system is more active while we sleep.
This also raises the question of whether good sleep might lead to better clearance of toxins such as Aβ from the brain, and so be a potential target to prevent dementia.
How about sleep apnoea or insomnia?
What is less clear is what long-term disrupted sleep, for instance if someone has a sleep disorder, means for the body’s ability to clear Aβ from the brain.
Sleep apnoea is a common sleep disorder when someone’s breathing stops multiple times as they sleep. This can lead to chronic (long-term) sleep deprivation, and reduced oxygen in the blood. Both may be implicated in the accumulation of toxins in the brain.
Sleep apnoea has also been linked with an increased risk of dementia. And we now know that after people are treated for sleep apnoea more Aβ is cleared from the brain.
Insomnia is when someone has difficulty falling asleep and/or staying asleep. When this happens in the long term, there’s also an increased risk of dementia. However, we don’t know the effect of treating insomnia on toxins associated with dementia.
So again, it’s still too early to say for sure that treating a sleep disorder reduces your risk of dementia because of reduced levels of toxins in the brain.
So where does this leave us?
Collectively, these studies suggest enough good quality sleep is important for a healthy brain, and in particular for clearing toxins associated with dementia from the brain.
But we still don’t know if treating a sleep disorder or improving sleep more broadly affects the brain’s ability to remove toxins, and whether this reduces the risk of dementia. It’s an area researchers, including us, are actively working on.
For instance, we’re investigating the concentration of Aβ and tau measured in blood across the 24-hour sleep-wake cycle in people with sleep apnoea, on and off treatment, to better understand how sleep apnoea affects brain cleaning.
Researchers are also looking into the potential for treating insomnia with a class of drugs known as orexin receptor antagonists to see if this affects the clearance of Aβ from the brain.
If you’re concerned
This is an emerging field and we don’t yet have all the answers about the link between disrupted sleep and dementia, or whether better sleep can boost the glymphatic system and so prevent cognitive decline.
So if you are concerned about your sleep or cognition, please see your doctor.
Julia Chapman, Clinical Trials Lead and Postdoctoral Research Fellow, Woolcock Institute of Medical Research and Conjoint Lecturer, Macquarie University; Camilla Hoyos, Senior Lecturer in the Centre for Sleep and Chronobiology, Macquarie University, and Craig Phillips, Associate Professor, Macquarie Medical School, Macquarie University
This article is republished from The Conversation under a Creative Commons license. Read the original article.