New Swedish Study Challenges Early Surgery for Crohn’s Disease

A new study from Karolinska Institutet challenges previous findings that suggested early surgery is more beneficial in the long term than medical treatment for patients with Crohn’s disease. The study replicates a Danish registry study using Swedish data and finds that the results are not comparable. The study was published in Clinical Gastroenterology and Hepatology.
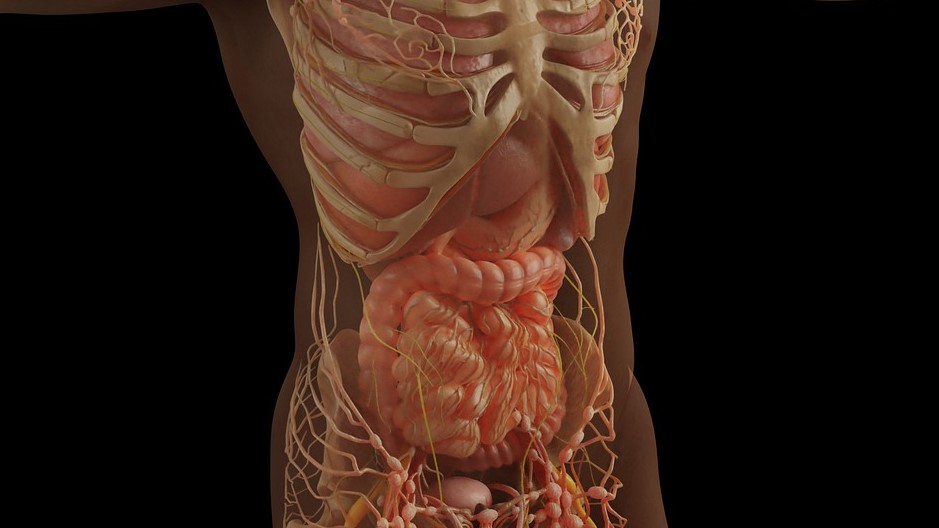
A few years ago, a randomised controlled trial showed that early ileocecal resection – removal of the junction between the small and large intestine – could be a reasonable alternative to advanced drug therapy for patients with Crohn’s disease. This study gained significant attention and was widely discussed around the world. Recently, a Danish research group published a registry-based study in the journal Gastroenterology, concluding that real-world data showed that early ileocecal resection was clearly superior to medical treatment in the long term.
In the new Swedish study, researchers attempted to replicate the Danish study using nationwide Swedish registry data. They found that it is impossible to identify comparable populations in current observational data, as patients who underwent surgery or received medication during the study period differ according to existing treatment guidelines.
“It’s a comparison of apples and oranges,” says Ola Olén, professor at the Department of Medicine, Solna, Karolinska Institutet, who led the study.
The Danish researchers made several design choices that further reduced the comparability between the groups. When the Swedish researchers applied the same definitions as the Danish study, they obtained similar results. However, when they used stricter definitions that more closely resembled the original randomized study, they no longer found a significant difference between the groups.
“We argue that the Danish study cannot be interpreted as proof that early surgery is better. That may very well be the case, but the data we currently have simply cannot answer that question,” says Ola Olén.
Source: Karolinska Institutet