Cipla Partners with ImmunoACT to Launch New CAR-T Cell Therapy for Blood Cancers in Africa
Cipla Limited (BSE: 500087; NSE: CIPLA; and hereafter referred to as “Cipla”), through its subsidiary Medpro Pharmaceutica, has entered into an exclusive license and supply agreement with Immunoadoptive Cell Therapy Private Limited (ImmunoACT). Under this partnership, Cipla will commercialise talicabtagene autoleucel, India’s first indigenously developed CAR-T cell therapy, in the Republic of South Africa, Algeria, and Morocco.
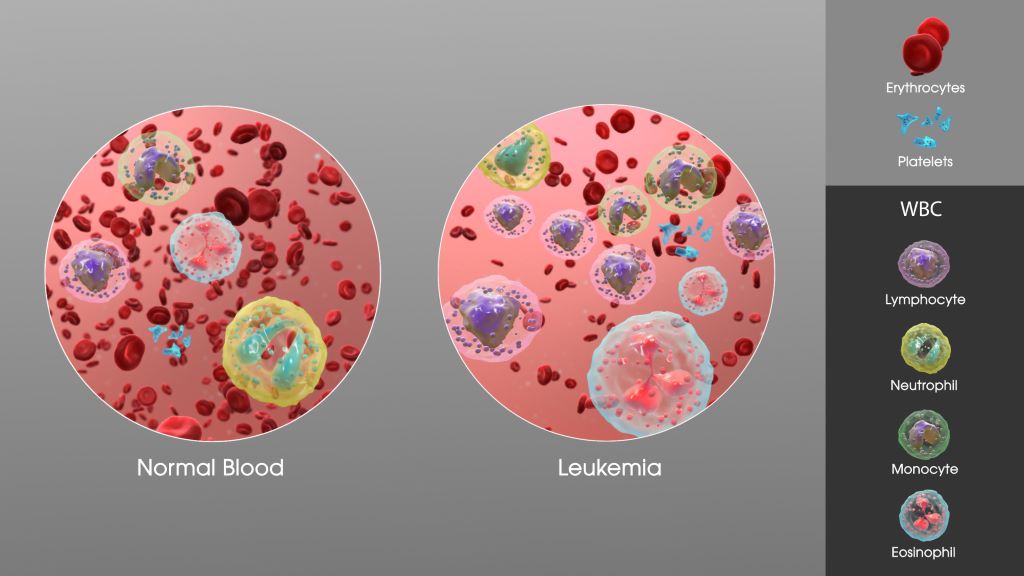
Talicabtagene autoleucel (the product) is an autologous (of a patient’s own blood sample) anti-CD19 CAR-T indicated for the treatment of patients with relapsed or refractory B-cell Non-Hodgkin’s Lymphoma (B-NHL) and B-cell Acute Lymphoblastic Leukaemia (B-ALL) who have failed standard lines of therapy. Administered to over 500 patients in India, the therapy has demonstrated high efficacy, durable responses, and a well‑tolerated safety profile, leading to reduced ancillary healthcare costs.
As part of this collaboration, ImmunoACT will manufacture the product and Cipla will commercialise in the licensed African territories, thereby expanding access of this revolutionary new treatment to markets currently with unmet needs.
Commenting on the partnership, Achin Gupta, Managing Director and Global CEO Designate, Cipla Limited, said, “Our collaboration with ImmunoACT reinforces Cipla’s vision of leveraging cutting-edge science to deliver transformative and affordable treatments, especially for patients with critical healthcare needs. By introducing CAR-T therapy in Africa, we aim to bring world-class innovation closer to patients and strengthen our commitment to accessible healthcare in the region.”
Adding on, Paul Miller, Chief Executive Officer of Cipla Africa, said, “We are proud to be at the forefront of efforts to bring CAR-T cell therapy to Africa. This collaboration not only advances our oncology portfolio but also reinforces Cipla’s mission of making next-generation therapies accessible to patients worldwide.”
Dr. Rahul Purwar, ImmunoACT’s Founder & Chairman and a professor of the Indian Institute of Technology (IIT), Bombay, said, “Our mission has always been to innovate and make cell & gene therapies accessible and affordable, addressing the significant unmet medical needs across the globe. This strategic partnership with Cipla seeks to accelerate our endeavours; ensuring that patients with B-cell cancers have a fighting chance at a durable remission, with our CAR-T platform.”
About CAR-T cell therapy:
CAR T-cell therapy is a groundbreaking form of immunotherapy that uses a patient’s own immune cells to fight the disease. Doctors collect immune cells (T cells) from the patient, reprogram them to identify and destroy cancer cells, and then return them to the body, enabling a targeted and personalized approach to treatment.
About Cipla
Established in 1935, Cipla is a global pharmaceutical company focused on agile and sustainable growth, complex generics, and deepening portfolio in our home markets of India, South Africa, North America, and key regulated and emerging markets. Our strengths in the respiratory, antiretroviral, urology, cardiology, anti-infective and CNS segments are well-known. Our 46 manufacturing sites around the world produce 50+ dosage forms and 1500+ products using cutting-edge technology platforms to cater to our 80+ markets. Cipla is ranked 3rd largest in pharma in India (IQVIA MAT Sep’25), 2nd Largest in the pharma prescription market in South Africa (IQVIA MAT Aug’25), and 4th largest by prescription in the US Gx (Repulses + MDI) products (IQVIA MAT Aug’25). For over nine decades, making a difference to patients has inspired every aspect of Cipla’s work. Our paradigm-changing offer of a triple anti-retroviral therapy in HIV/AIDS at less than a dollar a day in Africa in 2001 is widely acknowledged as having contributed to bringing inclusiveness, accessibility and affordability to the centre of the HIV movement. A responsible corporate citizen, Cipla’s humanitarian approach to healthcare in pursuit of its purpose of ‘Caring for Life’ and deep-rooted community links wherever it is present make it a partner of choice to global health bodies, peers and all stakeholders. For more, please visit www.cipla.com, or click on Twitter, Facebook, LinkedIn.
About ImmunoACT
As pioneers of India’s first fully integrated CAR-T cell therapy platform, ImmunoACT (Immunoadoptive Cell Therapy Private Limited), develops and manufactures accessible, affordable cutting-edge gene-modified cell therapies for blood cancers and solid tumours. With NexCAR19™, India’s first CAR_T cell therapy (developed in collaboration with the Indian Institute of Technology, Bombay and Tata Memorial Centre) commercially approved in India having unprecedentedly transformed the treatment landscape in refractory/relapsed B-cell malignancies, ImmunoACT also has a robust pipeline including a clinical-stage BCMA-directed CAR-T for multiple myeloma, and solid tumour CAR-Ts under development. The company is accelerating its mission to expand global access to life-saving cell and gene therapies through strategic partnerships.


