Vibration Technique Controls Strength of Lab-grown Tissues
Researchers in McGill’s Department of Mechanical Engineering have discovered a safe and low-cost method of engineering living materials such as tissues, organs and blood clots. By simply vibrating these materials as they form, scientists can dramatically influence how strong or, weak they become.
The findings, published in the journal Advanced Functional Materials, could have a range of innovative applications, including in organ transplants, wound healing and regenerative medicine.
Good vibrations
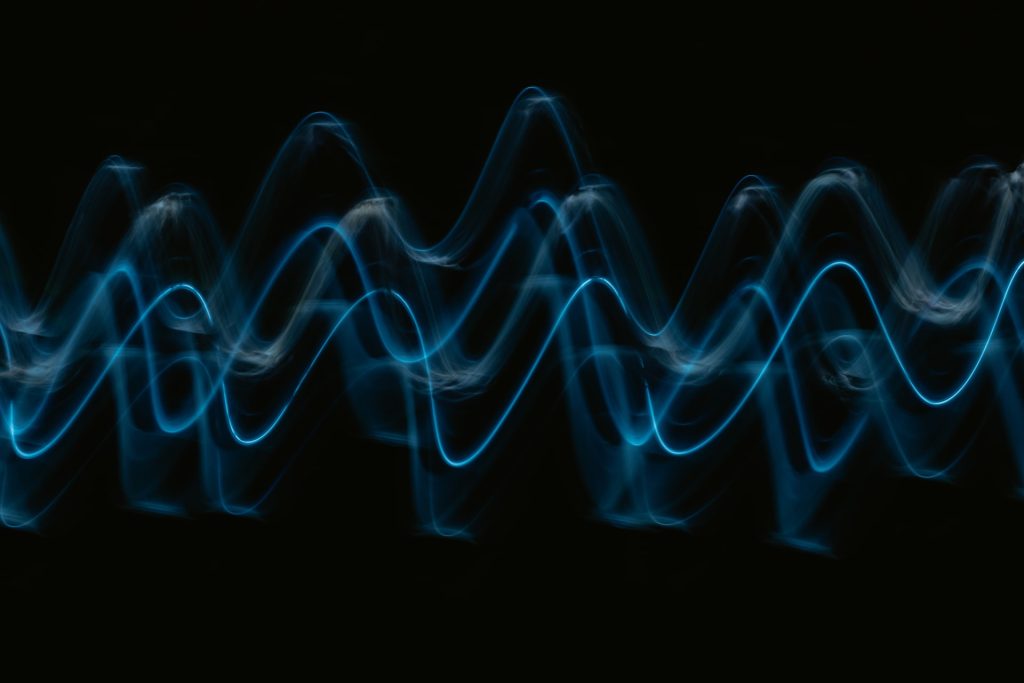
The researchers used a speaker to apply controlled vibration, gently agitating the living materials during formation. By doing so, they found they could influence how cells organized and how strong or weak the final material became.
The technique works across a range of soft cellular materials, including blood clots made from real blood and other human tissues.
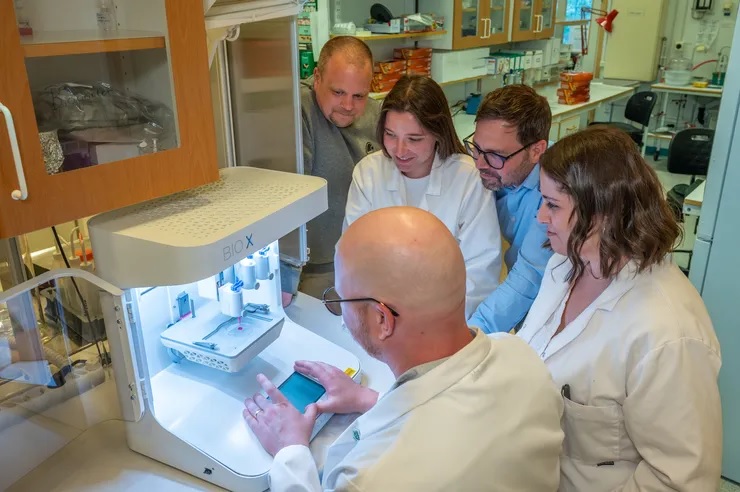
Aram Bahmani, study co-author and Yale postdoctoral fellow, conducted the research at McGill as a PhD student with Associate Professor Jianyu Li’s Biomaterials Engineering lab. Bahmani explained that strong, fast-forming blood clots are vital for use in emergencies like traumatic injuries. They’re also useful for people with clotting disorders.
“On the other hand, the same approach could help design clots that break down more easily as necessary, helping to prevent dangerous conditions like stroke or deep vein thrombosis,” he added. “Mechanical nudging allows us to make the material up to four times stronger or weaker, depending on what we need it to do.”
Why previous methods fell short
Earlier approaches to shaping living tissues relied on physical forces like magnets or ultrasound waves. While promising, these methods often fail to replicate the complexity of real tissues, which contain billions of cells and have thick, three-dimensional structures. In addition, they are often limited to specific materials, can damage healthy tissues and sometimes trigger immune responses.
The researchers’ study is the first to show that mechanical agitation, a very simple and widely accessible tool, can control the inner structure and performance of living materials in a “safe, scalable and highly tunable way.”
From the lab bench to living systems
To validate their findings, the team ran a series of tests to measure how vibration affected various cell-laden materials such as blood-based gels, plasma and seaweed-derived alginate. Using imaging and mechanical analysis, they assessed how broadly the method could be applied. Next, they tested the technique in animals.
The results showed that the technique works when applied inside the body, without harming surrounding healthy tissues.
Toward advanced medical technology
Bahmani said he believes the simple method could one day be integrated into advanced medical devices or wound-healing techniques.
“What makes this especially exciting is that our method is non-invasive, low-cost and easy to implement,” he said. “It does not rely on expensive machines or complex chemicals, meaning it could one day be built into portable medical devices, like a hand-held tool to stop bleeding, or a smart bandage that speeds up healing.”
He noted that the method requires further testing, such as in irregular wounds or in combination with certain medications, before it can be used in real-life medical settings.
“Moving toward clinical use will require miniaturising the devices, optimising settings for different medical scenarios and completing regulatory testing to ensure safety and effectiveness in humans,” he said.
Source: McGill University