Study Uncovers a Key Brain Building Block

A new study from Duke and UNC scientists has discovered a crucial protein involved in the communication and coordination between astrocytes as they build synapses — essentially a brain building block.
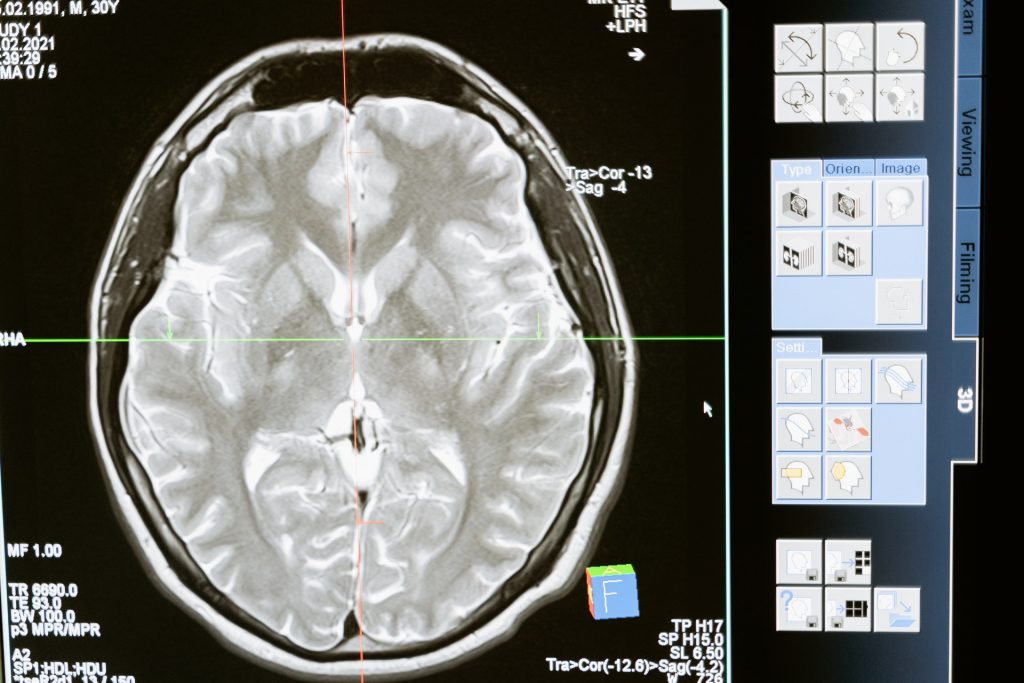
Astrocytes, specialised, star-shaped glial cells that outnumber the neurons they support over fivefold and which make up about half the mass of a human brain, are increasingly being viewed as having a critical role in shaping the development of the brain. Astrocytes tile the entire central nervous system (CNS) and exert many essential complex functions in the healthy CNS, including guiding development of the brain.
The researchers found that a molecule, called hepaCAM, is a key component of this process. Without it, astrocytes aren’t as sticky as they should be, and tend to stick to themselves rather than forming connections with their neighbouring astrocytes.
This finding, in studies on mice with the gene for hepaCAM deleted from their astrocytes, helps in the understanding of several brain disorders, including cognitive decline, epilepsy and autism spectrum disorders.
One rare brain disorder, called megalencephalic leukoencephalopathy (MLC) is also known to be caused by a mutation in the hepaCAM gene, and this work might provide answers about what exactly has gone wrong. MLC is a developmental disorder that grows progressively worse, causing macrocephaly (a large head), swelling of the brain’s white matter, intellectual disability and epilepsy.
By deleting hepaCAM from astrocytes to see what it does, “we sort of made the cells into introverts,” explained senior author Cagla Eroglu, an associate professor of cell biology at the Duke University School of Medicine. “They’re normally wanting to reach out, but without hepaCAM, they started to hug themselves instead.”
“If the astrocyte makes junctions to its neighbours, then you start to have a network,” Prof Eroglu said. “To make a functional brain, you need a functional astrocytic network.”
The researchers zeroed in on hepaCAM by searching for highly active genes in astrocytes, and which have been implicated in brain dysfunction. They partnered with another group working on hepaCAM at the University of Barcelona, but that group has been looking at the molecule for its role in regulating chloride signaling channels in astrocytes.
The Duke group found that deleting hepaCAM from astrocytes led to a synaptic network that was too easily excited and not as well dampened. “The effect on the inhibitory synapses was the strongest,” said first author Katie Baldwin, who recently became an assistant professor of cell biology and physiology at the University of North Carolina at Chapel Hill. “You’re putting the inhibition down and the excitation up, so that really could point to a mechanism for epilepsy.”
Prof Baldwin plans to test whether hepaCAM-deficient mice have behavioural differences or changes in learning and memory, or whether they exhibit the stress and social anxiety that are markers of autism spectrum disorders. She said they might also reintroduce the disease-mutation versions of the protein to mice that were born without it to see what effects it has.
“We know hepaCAM is interacting with itself between two astrocytes, but we don’t know what it’s interacting with at the synapse,” Prof Baldwin said. “We don’t know if it could be interacting with hepaCAM which is also found in the neurons, or if it could be some other protein that we don’t know about yet.
Source: Duke University School of Nursing
Journal information: Katherine T. Baldwin et al, HepaCAM controls astrocyte self-organization and coupling, Neuron (2021). DOI: 10.1016/j.neuron.2021.05.025