Radiotherapy Overcomes Resistance to Immunotherapy in Some Cancers
By sparking the immune system into action, radiation therapy makes certain tumours that resist immunotherapy susceptible to the treatment, leading to positive outcomes for patients, according to new research published July 22 in Nature Cancer. Investigators dove deep into the molecular biology of non-small cell lung cancer to pinpoint what happens on a cellular and molecular level over time when the cancer is treated with either radiation therapy followed by immunotherapy or immunotherapy alone.
They found that radiation plus immunotherapy induced a systemic anti-tumour immune response in lung cancers that do not typically respond to immunotherapy. The combination therapy also yielded improved clinical response in patients whose tumours harbour features of immunotherapy resistance.
Clinically, the results suggest that radiation therapy can help overcome immunotherapy resistance in certain patients. Researchers at the Johns Hopkins Kimmel Cancer Center Bloomberg~Kimmel Institute for Cancer Immunotherapy and the Netherlands Cancer Institute conducted the study, which was supported by the National Institutes of Health.
“For a fraction of lung cancers where we aren’t expecting therapy responses, radiation may be particularly effective to help circumvent primary resistance to immunotherapy; this could potentially be applicable to acquired resistance, too,” says senior study author Valsamo “Elsa” Anagnostou, MD, PhD, co-director of the Upper Aerodigestive Malignancies Program, director of the Thoracic Oncology Biorepository, leader of Precision Oncology Analytics, co-leader of the Johns Hopkins Molecular Tumor Board and co-director of the Lung Cancer Precision Medicine Center of Excellence at Johns Hopkins.
Researchers have long sought to better understand why some tumours grow resistant to immunotherapy and how to intercept that resistance.
Radiation therapy has been proposed as one possible way to induce a systemic immune response because of a unique phenomenon called the abscopal effect. Radiation at the site of a primary tumour typically causes tumour cells to die and release their contents into the local microenvironment. Sometimes, the immune system discovers those contents, learns the tumour’s molecular footprint, then activates immune cells around the body to attack cancer cells at tumour sites that were not the targets of the radiation, including some far away from the primary cancer in the body.
Because of this effect, radiation therapy could potentially improve how well an immunotherapy works against a cancer, even far from the original radiation site. Yet little has been known about the molecular biology behind the abscopal effect, or how to predict when and in which patients it will occur.
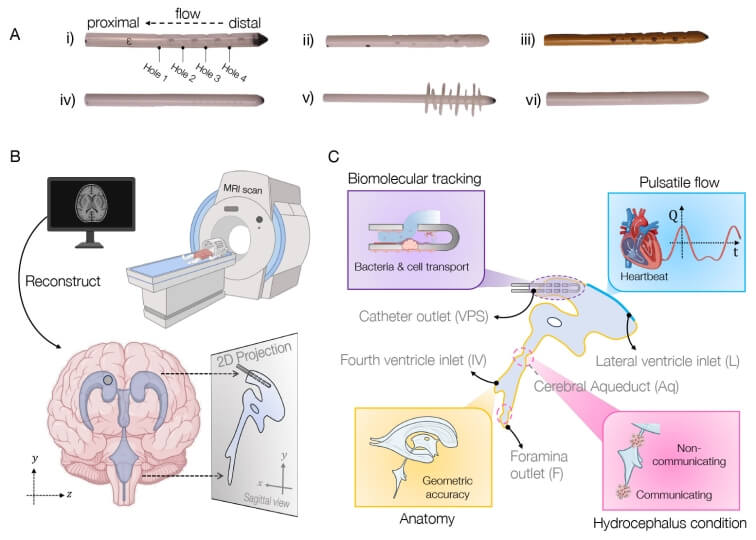
To study this phenomenon, Anagnostou and colleagues obtained samples from patients with lung cancer at different times throughout their treatment journey and from various locations in the body, not just at the primary tumour site. They collaborated with Willemijn Theelen and Paul Baas at the Netherlands Cancer Institute, who were running a phase II clinical trial on the effect of radiation therapy followed by immunotherapy, specifically the PD-1 inhibitor pembrolizumab.
With help from Theelen and Baas, Anagnostou’s team analysed 293 blood and tumour samples from 72 patients, obtained at baseline and after three to six weeks of treatment. Patients in the control group received immunotherapy alone, while the experimental group received radiation followed by immunotherapy.
The team then performed multiomic analyses on the samples (combining different “omics” tools, including genomics, transcriptomics and various cell assays) to deeply characterise what was happening to the immune system systemically and in the local microenvironment at tumour sites that were not directly exposed to radiation.
In particular, the team focused on immunologically “cold” tumours — those that typically do not respond to immunotherapy. These tumours can be recognised by particular biomarkers: a low mutation burden, no expression of a protein called PD-L1, or the presence of mutations in a signalling pathway called Wnt.
Following radiation and immunotherapy, the team found that “cold” tumors far from the site of radiation experienced a prominent reshaping of the tumor microenvironment. Anagnostou describes this shift as the tumors “warming up,” transitioning from little or no immune activity to inflamed sites with strong immune activity, including the expansion of new and pre-existing T cells.
“Our findings highlight how radiation can bolster the systemic anti-tumor immune response in lung cancers unlikely to respond to immunotherapy alone,” says lead study author Justin Huang, who led the multiomic analyses. “Our work underscores the value of international, interdisciplinary collaboration in translating cancer biology insights to clinical relevance.” Huang was awarded the 2025 Paul Ehrlich Research Award in recognition of groundbreaking discoveries by young investigators and their faculty mentors at the Johns Hopkins University School of Medicine.
With Kellie Smith, PhD, an associate professor of oncology at the Johns Hopkins Kimmel Cancer Center and a Bloomberg~Kimmel Institute for Cancer Immunotherapy researcher, Anagnostou’s team focused on patients who attained long-term survival with combination radiotherapy and immunotherapy, and performed a functional test to find out what the patients’ own T cells were doing in the body. In cell cultures, they confirmed that the T cells expanding in patients who received radiation and immunotherapy were indeed recognizing specific mutation-associated neoantigens from the patients’ tumours.
Finally, by tracking patient outcomes from the clinical trial, the team observed that patients with immunologically cold tumours that “warmed up” due to radiation therapy had better outcomes than those who did not receive radiation therapy.
“It was super exciting, and truly made everything come full circle,” says Anagnostou. “We not only captured the abscopal effect, but we linked the immune response with clinical outcomes in tumours where one would not expect to see immunotherapy responses.”
Using specimens from the same cohorts of patients, the team has recently been working to capture the body’s response to immunotherapy by detecting circulating tumour DNA (ctDNA) in the blood. That work was presented April 28 at the annual meeting of the American Association for Cancer Research in Chicago.
Source: Johns Hopkins Medicine