Zinc-based Compound Could be a New Cavity Fighter
Scientists at NYU are developing a zinc-based treatment for tooth decay that combats bacteria, blocks pain, and avoids staining teeth – all without drilling

Tooth decay is the most common health condition worldwide. While it is preventable and treatable, billions of people are living with cavities and the pain that accompanies them.
Given the massive scale of the problem, there’s a growing movement in dentistry to treat cavities without drilling and filling them. One such approach is applying a clear liquid called silver diamine fluoride to the surface of teeth. Silver diamine fluoride is already FDA-approved to treat tooth sensitivity, and recent NYU research shows that the compound’s antimicrobial properties also make it effective at preventing cavities and stopping small cavities from progressing into larger ones. Because it’s inexpensive and easy to administer, it can be given in schools, in rural areas lacking dentists, or to patients who may have difficulty with dental care, including those with disabilities.
But treatment with silver diamine fluoride comes with one notable drawback: when the silver in it interacts with tooth decay, it turns the treated surface black. While this is not a significant issue for molars at the back of the mouth or baby teeth that fall out, it’s not a great option for teeth seen in a smile.
“Once your teeth are treated with silver diamine fluoride, that stain is permanent, which is a barrier for many people wanting to use the product,” explains Marc Walters, professor of chemistry at NYU.
Walters has long studied silver and other elements used in medicine to carry drugs and imaging contrast agents. Several years ago, he was approached by researchers at NYU College of Dentistry seeking to better understand how silver stains teeth in order to avoid that outcome.
From silver to zinc
Walters had an idea. What if another mineral could be used that was also colourless and antimicrobial but didn’t turn teeth black? This question led him to zinc, an important nutrient found in foods like oysters and beef, as well as in over-the-counter products intended to shorten the duration of colds. Zinc is also used in dentistry, including in toothpaste and mouthwash to fight bacteria and bad breath, as well as in some denture adhesives and cementing agents to affix crowns or temporary fillings.
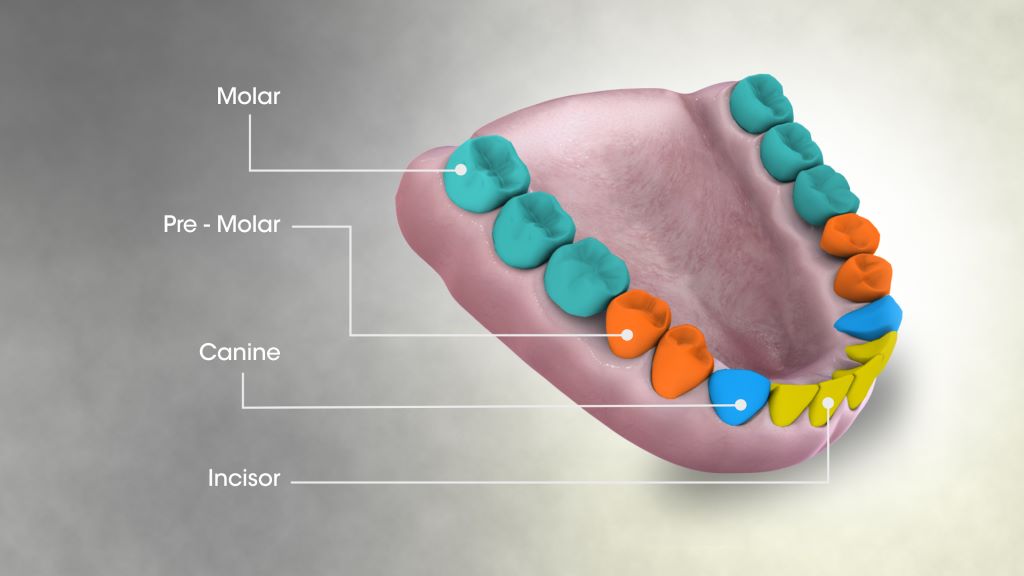
Walters began studying a zinc phosphate compound to see how it interacts with cavities, and crucially, to determine whether it can permeate deep into teeth. In order to address pain and hypersensitivity, the compound would need to reach the tooth’s dentin, the porous material sandwiched between the hard enamel outer layer and the nerves within. Dentin contains an abundance of microscopic, hollow channels – in fact, 40 000 of these tubules are packed into each square millimetre of dentin.
“We had to develop a solution to give dentists that will be taken up in these very small openings and go deep enough in the tubules so that the material will be retained,” Walters explains.
Walters applied phosphate followed by zinc to slices of a human tooth. Under the microscope, he saw deposits of the compound deep inside the dentin tubules. But while the zinc phosphate successfully permeated the teeth, he knew that a simpler approach that didn’t require applying two treatments would be easier for dentists. “Two steps is one too many,” says Walters.
Drawing inspiration from silver diamine fluoride, Walters developed another zinc-based molecule called zinc tetramine difluoride, which forms a colourless zinc oxide deep inside dentin tubules. The agent starts out as a liquid that is sensitive to concentration and pH. When painted onto a tooth and absorbed, the conditions within dentin tubules prompt a chemical change that quickly turns it into a solid, blocking the tubules and slowly releasing the antimicrobial zinc into the tooth.
His team is continuing to develop several related compounds for the treatment of cavities and has applied for patents of these zinc-based materials in several countries.
Fast and slow
Having both fact-acting and long-lasting properties would offer an ideal combination for fighting cavities and tooth sensitivity, given that many current treatments for sensitive teeth require multiple applications and can take days or weeks to work.
“In one of our studies, two minutes after treatment with our agent, we can see using the electron microscope that the zinc forms long cylinders of mineral that occupy the tubules,” says Walters. “Blocking the dentin tubules cuts off access to the nerves that are much deeper in dentin. It’s like putting a cork in place that shuts off the lower portion of the tubule from the outside environment – and this happens within a minute or two.”
Walters shows an image of a tubule under the microscope that was filled with the zinc compound.
In additional tests, Walters found that zinc oxide persisted in tooth samples for at least one to two months. The goal is to develop a product that lasts for months or even years inside of teeth, stopping hypersensitivity and fighting bacteria on an ongoing basis.
“Not only do you have the analgesic result of having tubules blocked, but you also have a very low solubility agent that can slowly release the zinc into the tubule to prevent the growth of Streptococcus mutans and other bacteria,” Walters adds.
The journey from lab to shelves
With a promising zinc nanocrystal agent in hand, Walters sought out other experts at NYU and beyond. His work caught the attention of Southern Dental Industries (SDI), an Australian company that makes restorative dental materials, including silver diamine fluoride. The company purchased the license for the zinc technology and NYU is working with them to develop it.
Closer to home, Walters began collaborating with Deepak Saxena, professor of molecular pathobiology and director of research innovation and entrepreneurship at NYU College of Dentistry.
Saxena and Walters are collaborating on a new NIH grant to further develop the zinc-based treatment.
As a result of bringing together this diverse expertise Saxena and Walters received a award from NYU, and last month, secured a grant from the NIH.
The NIH grant will fund feasibility studies for Walters’s team to further develop the formulation and confirm its ability to block tubules in a range of dentin samples. It will also fund research through Periomics Care in which Saxena’s team will study the agent’s antimicrobial properties. Specifically, they will look to see if the zinc creates a “zone of inhibition” – preventing the growth of decay-causing bacteria in the vicinity of it or even killing bacteria that comes in contact with it.
“The mouth is full of bacteria. A compound needs to have good antimicrobial activity, which can occur from ionic imbalance, the properties of the zinc, or by the fluoride,” Saxena says. “If a compound does not stain, has good antimicrobial activity, plus it blocks the tubules, then it should be successful in stopping tooth decay and be aesthetically accepted.”
Saxena and Walters are already planning for the next phase of their research, which will include additional studies on the compound’s formulation, effectiveness, toxicity, and shelf life. Ultimately, if these studies go well, the researchers and SDI will approach the FDA for permission to do a clinic trial.
One factor working in their favour: because zinc phosphate has long been used as a dental adhesive, it’s known to be safe and the FDA has already approved it in other forms. These existing products may pave the way for faster research and development of a cavity treatment compared to untested elements, which can take many years to develop.
The future of dentistry
A new non-invasive treatment for cavities could be a game-changer in oral health. “We know that there’s a need – and a market – for a product that stops tooth decay that is effective, cheap, easy to use, and non-staining, given the rise in global numbers of untreated cavities,” Saxena says.
Dentists could use it to treat cavities without needing to scrape or drill out the cavity in preparation. Squirmy kids would need less time in the dentist’s chair. Older adults who get cavities near the roots of their teeth as their gums recede could have a new option for stopping sensitivity and decay in difficult-to-treat areas. If safe and effective, perhaps small quantities could even be available on drugstore shelves and sold directly to consumers.
For Walters and Saxena, their goal is a future with less tooth decay and pain – and if their studies of zinc confirm its potential, silver-stained teeth may be a thing of the past.
Source: New York University