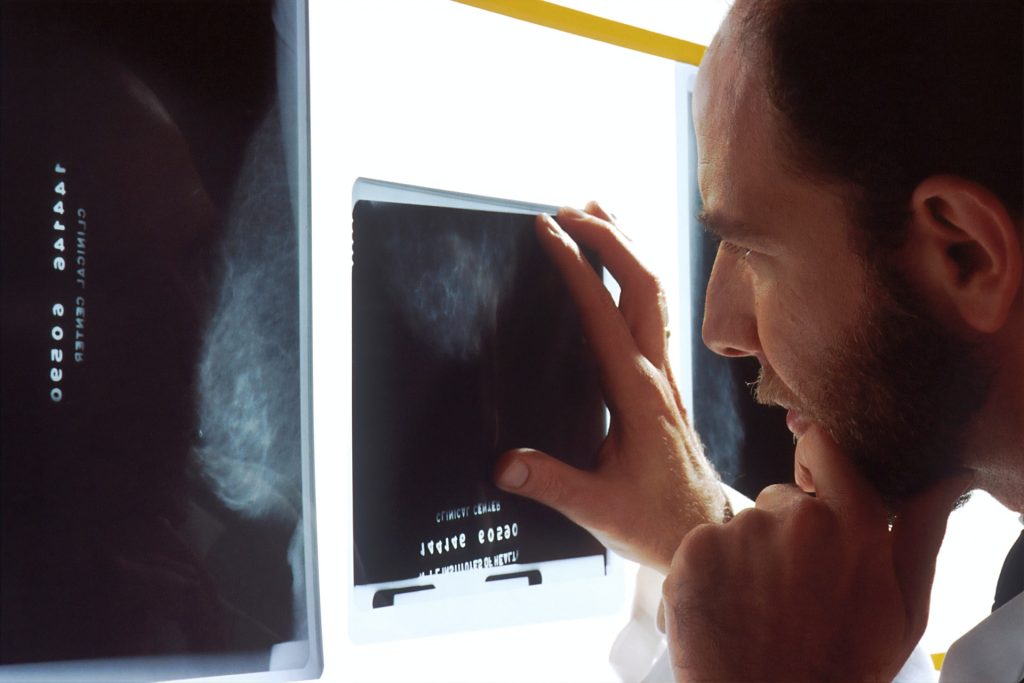
Radiotherapy After Mastectomy Can Be Avoided

Radiotherapy can be safely omitted as a treatment for many breast cancer patients who have had a mastectomy and are taking anti-cancer drugs, as shown in a study published in the New England Journal of Medicine. An international trial found that patients with early-stage breast cancer who underwent a mastectomy had similar 10-year survival rates whether or not they received radiotherapy.
Experts say the findings should help guide treatment discussions, as many patients who currently qualify for radiotherapy after mastectomy under existing guidelines may not actually need it.
Outdated practice
For many patients with early-stage breast cancer treated by mastectomy and anti-cancer drugs, chest wall radiotherapy has long been standard to kill any remaining cancer cells and lower the risk of recurrence.
The practice is based on trials from the 1980s, now considered outdated, leaving uncertainty about its benefit and leading to variation in use worldwide.
The SUPREMO trial (Selective Use of Postoperative Radiotherapy after Mastectomy), led by the University of Edinburgh, studied the impact of chest wall radiotherapy in patients at intermediate risk of breast cancer returning.
International trial
The group included women from 17 countries with one to three affected lymph nodes, as well as those with none but who had other tumour features of aggressive behaviour that increase the chance of recurrence.
All 1607 patients in the study underwent mastectomy, axillary surgery – removing lymph nodes from the armpit – and modern anti-cancer therapy. They were randomly assigned to chest wall radiotherapy (808 women) or no radiotherapy (799).
Little benefit
There was no difference in overall survival of patients after ten years of follow up – 81.4% of those who received radiotherapy were still alive, compared with 81.9% of those who did not.
Radiotherapy also had no impact on disease-free survival – the length of time without any cancer returning – or on the cancer spreading from the breast around the body, the study found.
Radiotherapy had minimal impact on cancer recurring at the site of mastectomy. Nine patients who received the treatment saw their breast cancer return on the chest wall, compared with 20 who did not. Side effects from radiotherapy were mild with no excess deaths reported from cardiac causes.
Improved drugs
Experts attribute radiotherapy providing less benefit than previously thought to progressive improvements in treatment, particularly better drug treatments, which continue to reduce the chances of the cancer returning, and boost survival rates.
The research team caution that the study only looked at those with intermediate-risk breast cancer. Patients with a higher risk of their cancer returning could possibly benefit from chest wall radiotherapy, they add.
The SUPREMO trial provides no evidence to support the continued use of radiotherapy to the area of the chest wall in most patients with intermediate-risk breast cancer who have undergone a mastectomy if they are also treated with modern anti-cancer drug treatment.
Professor Ian Kunkler Institute of Genetics and Cancer, University of Edinburgh
Although reported toxicity in the trial was mild, we know that almost all patients experience some side effects of radiotherapy, that can even develop even some years after treatment. Avoiding unnecessary irradiation will reduce both treatment burden and, for example, the detrimental effects on breast reconstruction for these mastectomy patients.
Dr Nicola Russell Netherlands Cancer Institute and study coordinator on behalf of the EORTC
The international research team included scientists from the UK, Netherlands, Australia and China.
Source: University of Edinburgh