The Current Gonorrhoea Meds Might Stop Working – When Will Newer Ones Make it to SA?
By Catherine Tomlinson
Two new antibiotics offer hope for people with gonorrhoea that is resistant to currently available drugs. Yet, it might be years before the people who need these medicines can get them. Spotlight unpacks why these new antibiotics are important and what needs to happen before they can be used in South Africa.
Gonorrhoea is a sexually transmitted infection known for its ability to quickly mutate to evade the antibiotics used to treat it. Its symptoms include pain when urinating and genital discharge, but many people don’t notice any symptoms at all. If gonorrhoea is not treated, it can cause serious problems including infertility, chronic pain and complications in babies who risk developing infections that can cause eye damage and blindness.
Gonorrhoea treatment has been something of a cat-and-mouse game as the bacteria continuously developed resistance against the antibiotics used to treat it. From the 1990s to the early 2000s, the antibiotic ciprofloxacin was used to treat gonorrhoea in South Africa, sometimes combined with another one called doxycycline. But as high levels of ciprofloxacin resistance emerged, South Africa replaced this course of therapy with a regimen of cefixime and doxycycline. Gonorrhoea treatment was changed again in 2015, due to concerns regarding the emergence of cefixime-resistance.
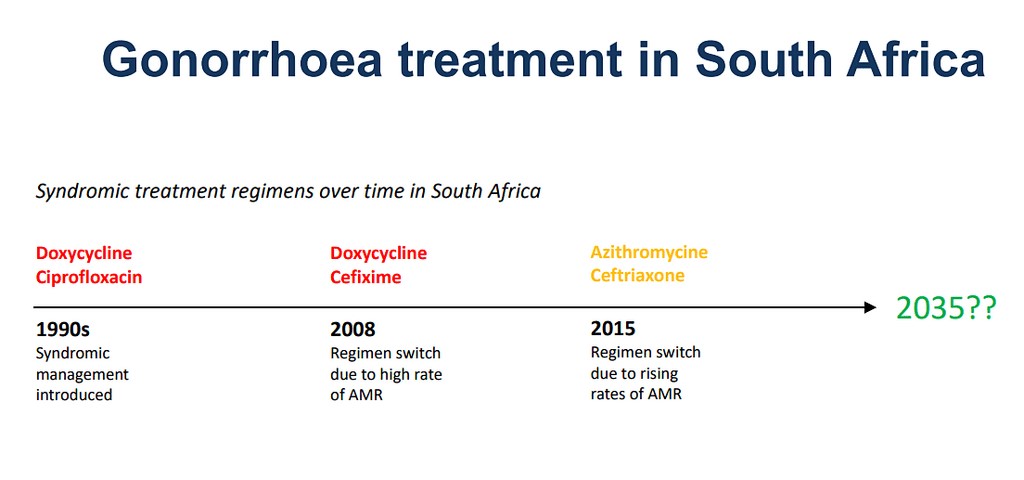
The treatment regimen adopted in 2015 remains the standard of care in South Africa and much of the world today. It involves an intermuscular injection of ceftriaxone, combined with oral azithromycin pills. Although, some countries now recommend using high dose injectable ceftriaxone on its own, due to high levels of azithromycin resistance.
While most gonorrhoea cases are still treatable with ceftriaxone, the emergence of ceftriaxone-resistant gonorrhoea has been identified as a major global health threat.
“The last effective drug we have, ceftriaxone, already indicates increasing gonococcal resistance. Without new antibiotics, we will have no easy treatment options. This is a great concern that will have a major impact in disease control efforts,” warned the World Health Organization (WHO).
This is why two new antibiotics, zoliflodacin and gepotidacin, are considered such a big deal. They are the first new medicines developed for gonorrhoea in over 30 years. Both are in new classes of antibiotics, which is to say they attack the bacterium in a different way than previous medicines. Because of this, they have little cross resistance with existing treatments and therefore offer important treatment options for people for whom the old medicines no longer work.
How widespread is ceftriaxone-resistance in South Africa?
How urgently we need access to the new medicines in South Africa will depend largely on how many people here are resistant to ceftriaxone. Unfortunately, we don’t have a clear picture of drug-resistant gonorrhoea in the country.
South Africa introduced a syndromic management approach for sexually transmitted infections (STIs) in the mid-1990s, as recommended by the WHO. This means that people reporting STI symptoms at health facilities are treated according to their symptoms, rather than results of a lab test.
This approach to STIs helps to reduce the cost burden of laboratory diagnosis and allows for immediate treatment initiation without waiting for laboratory results since some patients are “lost” over this period as they do not return to health facilities for their test results and treatment.
A challenge with treating STIs according to symptoms rather than laboratory results is that many STIs present with similar symptoms. This can lead to misdiagnosis and incorrect treatment as well as asymptomatic infections going undiagnosed and untreated.
Thus, without lab testing, combined with routine STI screening to identify asymptomatic cases, it is difficult to understand the true burden of gonorrhoea in the country or to measure the extent of drug resistance.
A systematic review, however, indicates that while azithromycin resistance is a challenge in South Africa, there was not yet evidence of ceftriaxone resistance as of 2022.
The National Institutes of Communicable Diseases (NICD) classified ceftriaxone-resistant gonorrhoea a notifiable condition in 2017, meaning that any diagnosed cases must be reported to it. The NICD did not respond to a query from Spotlight as to whether there have been any confirmed cases of ceftriaxone-resistant gonorrhoea in South Africa to date.
While South Africa is not yet facing a ceftriaxone-resistance crisis, experts are of the view that it is only a matter of time before this public health challenge reaches our borders, as global cases are increasing and the drug-resistant strain is transmittable.
Some access to zoliflodacin
Given the risk of a ceftriaxone-resistance crisis, it is important that the two new antibiotics, zoliflodacin and gepotidacin, become available here as soon as possible. These new antibiotics have quite different histories.
Zoliflodacin was developed by GARDP – a non-profit organisation working to accelerate the development of new antibiotics – together with the private biopharmaceutical company Innoviva.
In November 2023, GARDP shared the results of its phase 3 trial of zoliflodacin, which took place in South Africa, Thailand, Belgium, the Netherlands and the United States. It tested the effectiveness of a single dose of oral zoliflodacin compared with the current standard of care treatment for gonorrhoea, which is an injection of ceftriaxone combined with oral azithromycin.
The trial showed that a single dose of zoliflodacin works just as well as the standard of care. The results have not yet been published in a peer-reviewed journal.
Zoliflodacin has also “been shown to be active against all multidrug-resistant strains of Neisseria gonorrhoeae (the gonorrhoea bacteria), including those resistant to ceftriaxone, the last remaining recommended antibiotic treatment”, GARDP’s R&D Project Leader for STIs, Pierre Daram, told Spotlight.
He added that Innoviva is in the process of applying to get the greenlight to use zoliflodacin in the United States. At the same time, GARDP is planning to apply for approval in some of its own regions, starting with Thailand and South Africa.
GARDP is also working on a programme to make the unregistered drug available for patients who have no other treatment options.
“The zoliflodacin managed access programme is about to be activated,” Daram said. “The aim is to provide early access to zoliflodacin, prior to regulatory approval in a country, in response to individual patient requests by clinicians and whereby certain regulatory and clinical criteria are met.” South Africa will be one of the countries covered under this programme, said Daram.
He explained that individual patient requests for treatment will be received from treating clinicians through an online platform. “Based on information provided by the clinician and certain pre-determined regulatory and clinical criteria being met, GARDP will make a case-by-case decision as to whether zoliflodacin will be made available.” Daram added: “Consideration is given to both clinical as well as diagnostic criteria for documentation of treatment failure.”
Access to gepotidacin remains uncertain
Shortly after results for zoliflodacin were announced, GlaxoSmithKline (GSK) also shared positive findings for their new antibiotic in treating gonorrhoea. In April 2024, the company reported that a phase 3 trial showed that taking two doses of oral gepotidacin worked just as well as the standard treatment.
The results of this trial, which was conducted in Australia, Germany, Mexico, Spain, the United Kingdom, and the United States, were published in the Lancet medical journal in May.
While gepotidacin represents an important new treatment option for gonorrhoea, there is no indication that it will be available in South Africa any time soon.
Gepotidacin has not yet been registered for the treatment of gonorrhoea but was approved in March in the United States for treating uncomplicated urinary tract infections (UTIs) in women and girls over 12. The medicine will thus have a much larger market in the US than if it was only registered for treating gonorrhoea.
The price that GSK will charge for gepotidacin has not yet been disclosed, but a spokesperson told Spotlight it is set to be launched in the US in the second half of 2025.
“[T]he price in the US will be disclosed when the product will be commercialized,” said the GSK spokesperson.
The company did not respond to Spotlight’s questions regarding the company’s plans to register and market gepotidacin in South Africa.
What happens next?
With the launch of the zoliflodacin managed access programme, clinicians in South Africa will soon be able to apply for the medicine for patients that are resistant to existing drugs. Given that ceftriaxone-resistance is rare in the country, the number of patients in the country that will be eligible for zoliflodacin is likely to be small.
Securing broader access to zoliflodacin or gepotidacin, potentially for use as a first line gonorrhoea treatment appears to be a long way off. While GARDP is planning to file for registration of zoliflodacin in South Africa, GSK has not indicated whether they will follow suit for gepotidacin.
Providing the new antibiotics for first line gonorrhoea treatment could expand delivery and uptake, as the new drugs are both oral tablets and would remove the need for an injection to treat gonorrhoea, said Professor Nigel Garrett, who is the Chief Scientific Officer at the Desmond Tutu Health Foundation.
If zoliflodacin and gepotidacin are approved and made affordable in South Africa, they could also play a vital role in strengthening the country’s efforts to preserve the long-term effectiveness of other antibiotics.
Ceftriaxone “is a really important drug to keep, [to] make sure that there isn’t too much resistance against it,” Garret told Spotlight. He explained that the medicine is needed to treat sepsis occurring in hospitals, as well as meningitis.
Republished from Spotlight under a Creative Commons licence.
Read the original article.

