‘It’s a great sign’: Innovative Cochlear Implant Trial Expands Earlier than Expected

A highly sought-after clinical trial testing completely under-the-skin cochlear implants is expanding earlier than expected. Promising preliminary results showed no serious adverse events or unexpected device effects.
The Medical University of South Carolina, which has one of the larger cochlear implant programmes in the country, is one of several sites in the United States taking part in the Acclaim study. Three patients were implanted in the first wave of the trial and have been using their devices for at least six months. Now, MUSC has the chance to enrol more.
“New patients are coming this week, and we’re going to resume device placement as soon as possible. We have people flying in from all over the country to be part of the trial as well as South Carolinians,” said Teddy McRackan, MD He’s medical director of the MUSC Health Cochlear Implant Program.
Some participants are traveling to Charleston to get the experimental implants because slots in the 56-person national trial are limited, and they like the idea of cochlear implants without external parts.
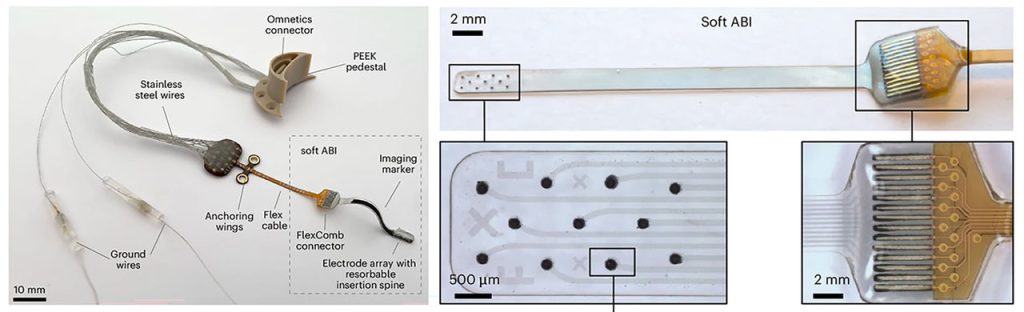
The Acclaim implants would be the first such devices to hit the market if they obtain approval from the Food and Drug Administration. McRackan said they use the body’s natural hearing bone movements to detect sound instead of the external microphones used in traditional cochlear implants.
“The trial has made it clear that hidden cochlear implants appeal to a lot of people,” said audiologist Elizabeth Camposeo, AuD. She’s assistant director of the MUSC Health Cochlear Implant Program.
“Seeing our patients going through this trial just feels like such a massive opportunity. I didn’t know how hard we were struggling to overcome the physical stigma of visible implants. There were many patients we screened for the trial who we could help with a traditional implant but who did not want any part of it. These people are profoundly hearing impaired, like 10 out of 10 terrible hearing, and they absolutely would not consider a traditional implant.”
They have plenty of company. Just 5% of adults in the United States who could hear better with traditional cochlear implants have them, according to the American Cochlear Implant Alliance.
To measure the Acclaim implants’ effectiveness, participants will check in for testing at one month, three months, six months, one year and two years after their implants are activated. Implantation requires surgery and then one month for healing before doctors turn on the devices.
Once the implants are activated, Camposeo said researchers will start analysing data about how much sound they detect and how well patients understand speech. “Similar to when you have your eyes checked, how close are you to 20/20 vision, we check sound detection. More importantly, we test speech understanding. We play a word. You repeat it back. We play a sentence. You repeat it back in both quiet and noise, because the world is a noisy place.”
A noisy place, and a place where potentially groundbreaking devices can be developed quickly, McRackan said. “I don’t think anybody thought two years ago that the Acclaim device would be at this point now. I think it’s kind of amazing how fast things are progressing.”