World Atopic Eczema Day 2025 calls for early intervention, better care, and greater awareness of the hidden toll of atopic dermatitis.
On 14 September, people around the world marked World Atopic Eczema Day 2025 under the theme: “Our Skin, Our Journey.” This year’s campaign highlights the lifelong nature of atopic eczema, also known as atopic dermatitis (AD), a disease that usually begins in infancy and can progress to food allergies, asthma and allergic rhinitis.1
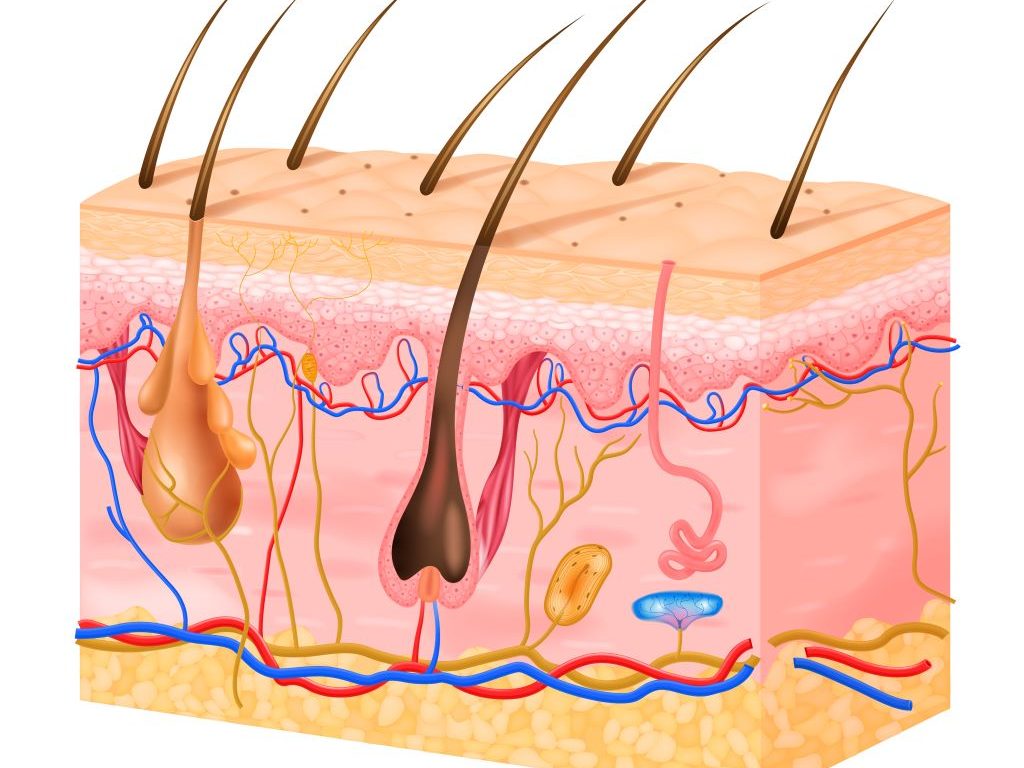
“Atopic eczema is more than a skin condition, it is driven by a dysregulated immune system and may have long-term physical and psychological impacts, and creates significant costs for families and healthcare systems,” says Dr Dwayne Koot, pharmacologist and Medical Advisor at Sanofi South Africa.
A disease that begins early
Atopic eczema is one of the most common chronic inflammatory skin diseases, affecting up to 20 percent of children globally.1 It often appears early in life. Around 45 percent of children with atopic eczema develop symptoms before six months of age, 60 percent before one year, and up to 85 percent before five years.1 For many, atopic eczema is the first step in what researchers call the “atopic march,” the progression from skin barrier dysfunction to food allergies and respiratory diseases.2
Studies show that infants with atopic eczema are six times more likely to develop egg allergy and eleven times more likely to develop peanut allergy than infants without atopic eczema.3 By later childhood, as many as 40 percent of children with atopic eczema develop food allergies.2 The condition does not stop there. School-age children with early, persistent atopic eczema face higher risks of developing asthma and allergic rhinitis.4
Beyond the skin
Atopic eczema is now recognised as a systemic disease linked to type 2 inflammation.1 The hallmark symptoms are itching, dry and inflamed skin, recurrent infections and disturbed sleep. These symptoms are not only uncomfortable but also disruptive to daily life.2,5
“Children may struggle at school due to fatigue, and parents often miss work or are unproductive due to sleepless nights, medical appointments or caring for their sick child,” says Dr Koot. “Because atopic eczema is so visible, children often face stigma. Studies show they are more likely to experience anxiety, depression and bullying. Up to one in three children with atopic eczema have anxiety or depression, compared with far fewer children without the disease.”
The economic impact is significant. In South Africa, while direct healthcare costs are relatively low (0,2 percent of healthcare spend), the total burden may be substantial when adding the much higher indirect costs and quality-of-life impacts.6
Why early intervention matters
While research is ongoing, one study found that daily use of emollients from birth to protect the skin barrier may lower the risk of eczema by half for high-risk infants, with no safety concerns.7
Additional research shows that the skin barrier is key in both atopic eczema and food allergies and protecting it early in life may help prevent these conditions.3 While allergen avoidance is still the main approach, new options like immunotherapy and biologics are showing promise.3
Recent findings emphasize that taking early, proactive action with advanced treatments can dramatically improve outcomes for patients, potentially changing the very course of this chronic skin condition.8,9
Traditionally, atopic eczema management has focused on treating symptoms as they arise, especially with topical creams for milder cases.8 However, a deeper understanding of the disease and the development of novel systemic treatments – medications that work throughout the body – reveal a powerful opportunity to intervene much earlier.8 This forward-thinking strategy moves beyond simply reacting to flare-ups; it aims to target the underlying immune imbalance and inflammation that drive eczema from its earliest stages.8
One of the most significant benefits of this early approach is its potential to halt the “atopic march”.9 This refers to the common progression where atopic eczema, often appearing first in infancy or childhood, is followed by other allergic conditions such as food allergies, allergic rhinitis, or asthma.9 By addressing the skin barrier dysfunction and immune system changes early on, we may be able to prevent or reduce the development of these related allergies.9 Studies suggest that allergic sensitization can occur through an impaired skin barrier, and early treatment of this dysfunction could serve as a preventive strategy for food allergy progression.9
Furthermore, early intervention is key to breaking the relentless “itch-scratch cycle”.8 Chronic itching, a hallmark of atopic eczema, not only causes immense discomfort but also leads to skin damage and secondary complications like infections. 8 By addressing the root causes of itching, patients can experience comprehensive relief, regain normalcy, and significantly improve their overall quality of life, sleep, and mental well-being by reducing anxiety, depression, and social isolation associated with the disease.8
This proactive strategy also offers the promise of long-term disease control and modification.8 By tackling inflammation before visible skin lesions fully develop, it can inhibit the escalation of inflammatory responses and disrupt the recurring cycles of flares and remissions.8
“The paradigm shift towards early systemic intervention represents a pivotal moment in atopic eczema care,” says Dr. Koot. “It’s about empowering patients with strategies that offer not just immediate relief, but also the potential for sustained positive outcomes and a better quality of life by addressing the disease at its inception, rather than solely managing its symptoms after they become severe.”
Working together
“World Atopic Eczema Day 2025 is a call to action,” says Dr Koot. “Doctors need to see atopic eczema as a systemic disease that needs more than just symptom relief. Policymakers need to support early treatment, better access to specialist care, affordable medicines, and stronger investment in research and innovation. Families and patient groups play a key role in showing the true impact of atopic eczema and pushing for advanced, targeted therapies.”
The campaign also recognises the importance of community. Social media initiatives such as #AtopicEczemaJourney give patients and families a space to share their stories, connect with others and draw attention to the reality of living with atopic eczema.
“Progress is possible, but it requires commitment from everyone,” says Dr Koot. “Research shows that simple measures, such as protecting infant skin with frequent use of emollients and avoiding triggers, can drastically improve control of atopic eczema. Public health strategies, better access to care, early intervention and investment in new treatments all make a difference. At the same time, society needs to understand that atopic eczema is not only about rashes or itching. It is a systemic, lifelong condition that affects education, careers, relationships and quality of life.”