Amazing Images Show How Antibiotics Shred Bacterial Armour
UK researchers have shown for the first time in stunning detail how life-saving antibiotics act against harmful bacteria. The team, led by UCL and Imperial College London, has shown for the first time how a class of antibiotics called polymyxins are able to pierce the armour of E. coli and kill the microbes.
The findings, published in the journal Nature Microbiology, could lead to new treatments for bacterial infections – especially urgent since drug-resistant infections already kill more than a million people a year.
Polymyxins were discovered more than 80 years ago and are used as a last-resort treatment for infections caused by “Gram negative” bacteria.
These bacteria have an outer surface layer that acts like armour and prevents certain antibiotics from penetrating the cell. Polymyxins are known to target this outer layer, but how they disrupt it and then kill bacteria is still not understood.
Through capturing these incredible images of single cells, we’ve been able to show that this class of antibiotics only work with help from the bacterium, and if the cells go into a hibernation-like state, the drugs no longer work – which is very surprising
Dr Andrew Edwards Department of Infectious Disease
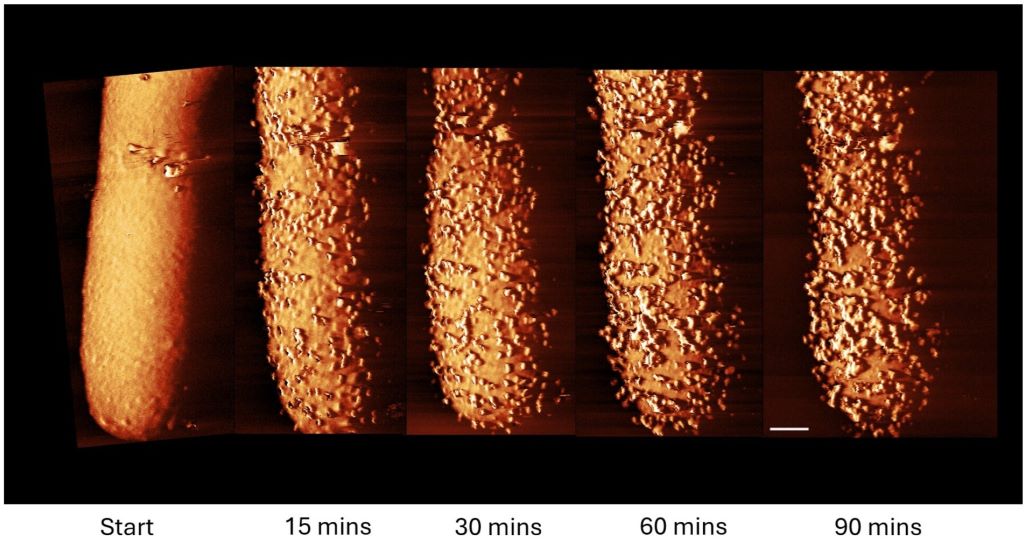
In the new study, the research team revealed in high-resolution images and biochemical experiments how the antibiotic Polymyxin B rapidly caused bumps and bulges to break out on the surface of an E. coli bacterial cell.
These protrusions, which appeared within minutes, were followed by the bacterium rapidly shedding its outer armour.
The antibiotic, the researchers concluded, had triggered the cell to produce and shed its armour.
The more the cell tried to make new amour, the more it lost the amour it was making, at such a rate that it left gaps in its defences, allowing the antibiotic to enter the cell and kill it.
However, the team found that this process – protrusions, fast production and shedding of armour, and cell death – only occurred when the cell was active. In dormant (sleeping) bacteria, armour production is switched off, making the antibiotic ineffective.
Co-senior author Dr Andrew Edwards, from the Department of Infectious Disease at Imperial College London, said: “For decades we’ve assumed that antibiotics that target bacterial armour were able to kill the microbes in any state, whether they’re actively replicating or they were dormant. But this isn’t the case.
“Through capturing these incredible images of single cells, we’ve been able to show that this class of antibiotics only work with help from the bacterium, and if the cells go into a hibernation-like state, the drugs no longer work – which is very surprising.”
Becoming dormant allows bacteria to survive unfavourable conditions such as a lack of food. They can stay dormant for many years and “wake up” when conditions become more favourable. This can allow bacteria to survive against antibiotics, for instance, and reawaken to cause recurrent infections in the body.
Co-senior author Professor Bart Hoogenboom, based at the London Centre for Nanotechnology at UCL, said: “Polymyxins are an important line of defence against Gram-negative bacteria, which cause many deadly drug-resistant infections. It is important we understand how they work.
“Our next challenge is to use these findings to make the antibiotics more effective. One strategy might be to combine polymyxin treatment – counterintuitively – with treatments that promote armour production and/or wake up ‘sleeping’ bacteria so these cells can be eliminated too.
“Our work also shows we need to take into account what state bacteria are in when we are assessing the effectiveness of antibiotics.”
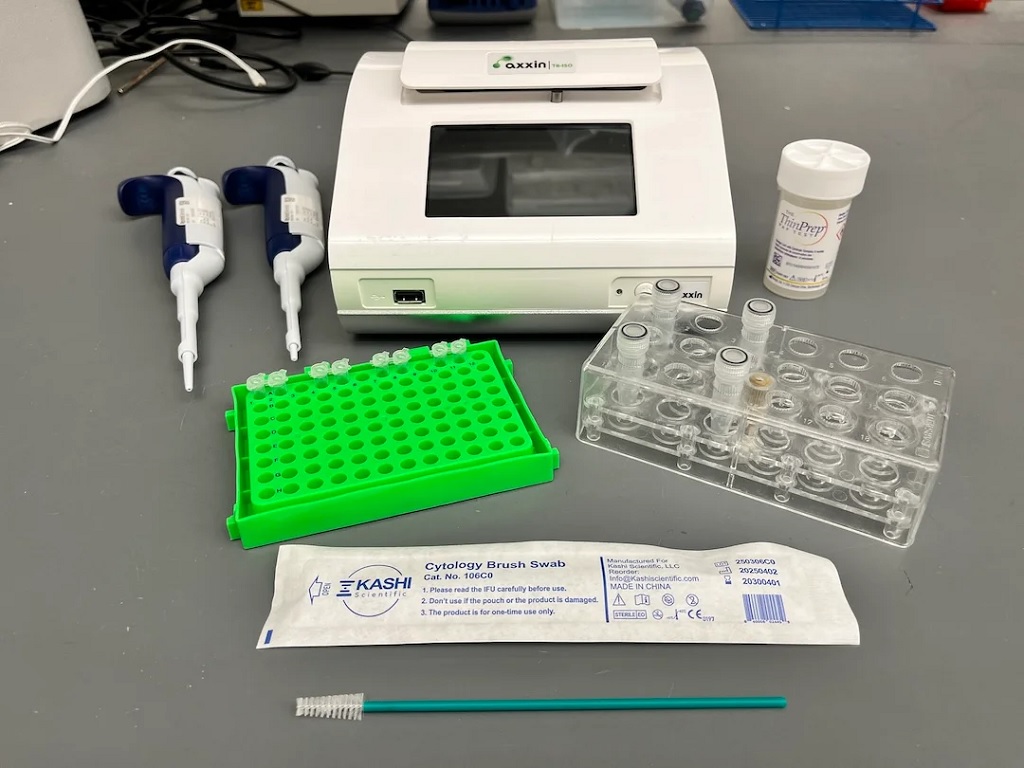
The E. coli cells were imaged at the London Centre for Nanotechnology at UCL. A tiny needle, only a few nanometres wide, was run over the bacterial cell, “feeling” the shape to create an image (a technique called atomic force microscopy) at much higher resolution than would be possible using light.
Co-author Carolina Borrelli, a PhD student at the London Centre for Nanotechnology at UCL, said: “It was incredible seeing the effect of the antibiotic at the bacterial surface in real-time. Our images of the bacteria directly show how much polymyxins can compromise the bacterial armour. It is as if the cell is forced to produce ‘bricks’ for its outer wall at such a rate that this wall becomes disrupted, allowing the antibiotic to infiltrate.”
The team compared how active (growing) and inactive E. coli cells responded to polymyxin B in the lab, finding that the antibiotic efficiently eliminated active cells but did not kill dormant cells.
They also tested the E. coli cells’ response with and without access to sugar (a food source that wakes up dormant cells). When sugar was present, the antibiotic killed previously dormant cells, but only after a delay of 15 minutes – the time needed for the bacteria to consume the sugar and resume production of its outer armour.
In conditions where the antibiotic was effective, the researchers detected more armour being released from the bacteria. They also observed the bulges occurring across the surface of the cell.
In conditions where it was ineffective, the antibiotic bound itself to the outer membrane but caused little damage.
Co-author Dr Ed Douglas, from Imperial, said: “We observed that disruption of the outermost armour of the bacteria only occurred when the bacteria were consuming sugar. Once we knew that, we could quickly figure out what was happening.”
Co-author Professor Boyan Bonev, of the University of Nottingham, said: “Working together has given us unique insights into bacterial physiology and morphology under stress that have remained hidden for decades. Now we understand better the weak points of bacteria.”
Source: Imperial College London