Salk Institute scientists uncover key role of kidneys in clearing inflammation from body, and show amino acid supplementation boosts this effect in mice
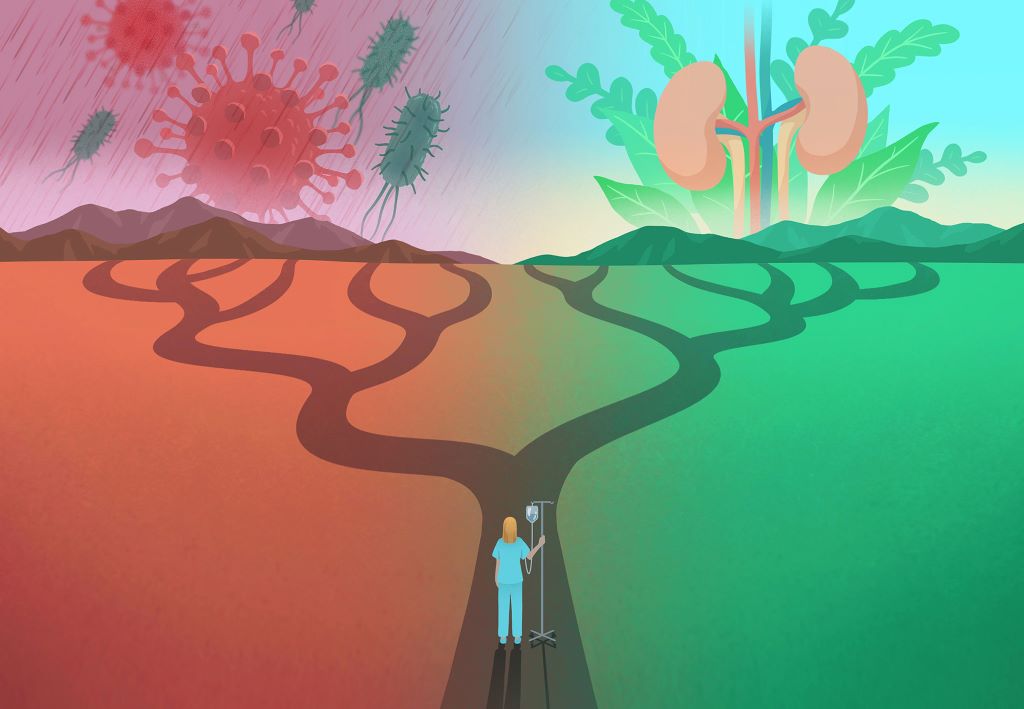
Disease trajectory is a unique journey from injury or infection, mediated by variable symptoms toward either recovery or death. It varies from person to person based on history, sex, age, and many other factors. Salk scientist Janelle Ayres, PhD, has spent decades unravelling the ways the body directs this journey – why some get sick and die while others go unscathed, and what sorts of methods could be used to shift trajectories of disease and death to ones of health and survival.
For many, inflammation is the ultimate cause of a downward trajectory toward death. Inflammation is a double-edged sword: a powerful weapon against intruders but an equally powerful generator of bodily damage if not properly regulated.
Since infections are some of the strongest drivers of inflammation-induced damage, the Salk team used a mouse model of infection to find that dietary supplementation of the amino acid methionine protected infected mice against inflammation-related wasting, blood-brain barrier dysfunction, and death. Methionine was accomplishing all this by boosting kidney filtration, revealing an underappreciated role the kidneys play in a successful journey from infection back to health.
The findings, published in Cell Metabolism on January 22, 2026, reveal the big impact that small dietary tweaks can have on disease trajectory, lighting the way to therapeutic strategies that steer patients from death to recovery. Methionine supplementation may be a useful tool for a variety of inflammatory conditions, as well as for patients with kidney disease or failure, or those undergoing dialysis.
“Our study indicates that small biological differences, including dietary factors, can have large effects on disease outcomes,” says senior author Ayres, professor and holder of the Salk Institute Legacy Chair at Salk, as well as a Hughes Medical Institute Investigator. “Our discovery of a kidney-driven mechanism that limits inflammation, together with the protective effects of methionine supplementation in mice, points toward the potential of nutrition as a mechanistically informed medical intervention that can direct and optimise the paths people take in response to insults that cause disease.”
Shifting the focus on inflammation
Research on the balance between too much and too little inflammation has been tricky, and mainly focused on how inflammatory responses are switched on and off. Ayres’s team is shifting the focus from these binary on/off mechanisms to studying how the body toggles the immune response higher or lower through the release and accumulation of pro-inflammatory cytokines.
“Pro-inflammatory cytokines are ultimately what leads to sickness and death in a lot of cases,” says first author Katia Troha, PhD, a postdoctoral researcher in Ayres’s lab. “The immune system has to balance inflammation to attack the invader without harming healthy cells in the body. Our job is to find the mechanisms it uses to do that, so that we can target them to improve patient outcomes.”
How can kidney function help reduce inflammation?
To understand how the body regulates its cytokine levels, the researchers used a mouse model of systemic inflammation induced by the pathogen Yersinia pseudotuberculosis. The first thing they noticed was that the infected mice were not eating as much – a sign of likely metabolic changes. To look at the nutritional status, the researchers looked at the levels of circulating amino acids, which are protein building blocks that support cellular health throughout the body.
Infected mice showed depressed methionine levels – an essential amino acid found in our everyday diets. Curious, Troha decided to feed a new batch of mice with methionine-supplemented chow, and surprisingly, these mice were protected against the infection.
Further experiments showed that methionine reduced circulating cytokine levels by partnering with a surprising ally: the kidneys. Methionine increased the kidneys’ filtration capacity, improving blood flow and helping the body excrete pro-inflammatory cytokines through the urine. Importantly, this methionine-kidney effect cleared excess cytokines without hindering other key aspects of the immune response.
Curious whether methionine’s effect was present in other conditions, the researchers also looked at sepsis and kidney injury models. They found that methionine was also protective for these mice, supporting that methionine may be a useful tool in other inflammatory disease settings.
Can dietary changes boost kidney performance?
By supplementing their diets with methionine, Salk scientists were able to give infected mice entirely different disease trajectories. The amino acid boosted the animals’ kidney function and protected them against wasting, blood-brain barrier dysfunction, and death without hindering their bodies’ ability to fight and kill Yersinia pseudotuberculosis.
And the sepsis and kidney injury models show these effects extend to other infections and inflammatory conditions, too, making methionine a potentially useful tool for the treatment of infectious diseases, particularly in cases of kidney disease or failure, or for patients undergoing dialysis.
“Our findings add to a growing body of evidence that common dietary elements can be used as medicine,” says Ayres. “By studying these basic protective mechanisms, we reveal surprising new ways to shift individuals that are fated to develop disease and die onto trajectories of health and survival. It may one day be possible for something as simple as a supplement with dinner to make the difference between life and death for a patient.”
While the results are promising, the researchers note that efficacy in humans is yet to be tested. Follow-up studies will explore the mechanisms by which methionine acts, whether other amino acids have similar or complementary effects, and how this may all translate to humans.
Source: Salk Institute

