Adaptive Spine Board Could Revolutionise ER Transport

In combat zones and emergency rescues, rapid evacuation and treatment can mean the difference between life and death. But prolonged immobilisation during transport poses another life-threatening risk: pressure injuries.
A newly developed adaptive spine board (ASB) overlay aims to change that, offering an innovative solution to prevent pressure injuries and dramatically improve patient outcomes. Developed by researchers at The University of Texas at Arlington and UT Southwestern Medical School, the adaptive spine board sits atop a standard stretcher or spine board, using air-cell technology to redistribute pressure more effectively than traditional evacuation surfaces. The team’s newly published study in the Journal of Rehabilitation and Assistive Technologies Engineering shows the ASB outperforms other immobilisation options.
“The ability to dynamically adjust pressure so that no vulnerable body regions experience excessive weight is a breakthrough for medical evacuation,” said Muthu B.J. Wijesundara, principal research scientist at the University of Texas at Arlington Research Institute. “This innovation could set a new standard in casualty transport protocols.”
Also called bedsores or ulcers, pressure injuries result from prolonged pressure on the skin and underlying soft tissue, leading to cell death, tissue breakdown and open wounds. They are a constant risk for trauma patients during long-range transport, which sometimes lasts more than 16 hours. Research shows that more than 50% of casualties transported during the Iraq War developed pressure injuries before reaching a hospital.
While some existing technologies, such as vacuum spine boards, can help redistribute pressure, their effectiveness is limited. Many conventional supports fail to keep pressure below the thresholds recommended to prevent injury. Military stretchers and pads have shown to create high-pressure points on vulnerable areas of the body, including the back of the head, base of the spine, buttocks and heels.
“Beyond military use, the ASB overlay could prove valuable in civilian medical transport, particularly for spinal injury patients who are at high risk for pressure ulcers,” Dr Wijesundara said. “The research also highlights potential applications in other environments where prolonged immobilisation is necessary, such as disaster relief and space exploration.”
The ASB overlay features a multi-segmented air-cell design that target pressure-prone areas more effectively than previous solutions. It is divided into five distinct sections—head and neck, upper trunk, buttocks and pelvis, thighs, and feet and heels—each equipped with sensor-driven pressure modulation for responsive, localised support.
“One key innovation is the system’s ability to autonomously adjust the air-cell pressure to maintain optimal distribution for each patient,” Wijesundara said. “We developed an algorithm that compensates for environmental variables, such as temperature and barometric pressure changes, ensuring consistent performance across varying conditions. Testing showed that the ASB overlay outperformed typical equipment used in casualty transport.”
For critically injured patients, pressure injuries can significantly complicate treatment and recovery, leading to longer hospital stays, higher infection risks and additional surgeries. They’re also costly. The Agency for Healthcare Research and Quality (AHRQ) estimates that pressure injuries in the US can cost up to $151 700 per case, adding $11.6 billion in additional health care expenses annually. Alarmingly, the AHRQ also reports that approximately 60 000 patients die each year because of pressure injuries. The ASB overlay’s advanced pressure modulation could help mitigate these risks—especially for patients who cannot be repositioned during extended transport.
The research team is now planning additional studies to improve the device’s usability in real-world conditions. As the military increasingly relies on prolonged aeromedical evacuation, such advancements are critical for enhancing patient care in conflict zones.



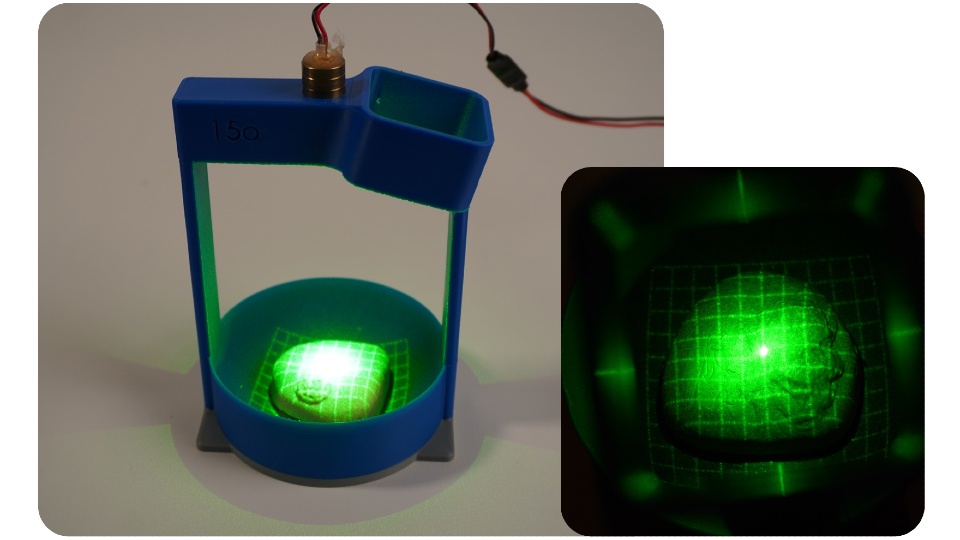 PRO check prototype one demonstrated how laser gridlines and a camera can be used to image the surface of the prostate.
PRO check prototype one demonstrated how laser gridlines and a camera can be used to image the surface of the prostate.

