New Nanomedicine Turns Toxic Chemo Drug into a Cancer Assassin
By restructuring a common chemo drug, scientists boost its power by 10 000-fold
In a promising advance for cancer treatment, Northwestern University scientists have re-engineered the molecular structure of a common chemotherapy drug, making it dramatically more soluble and effective and less toxic.
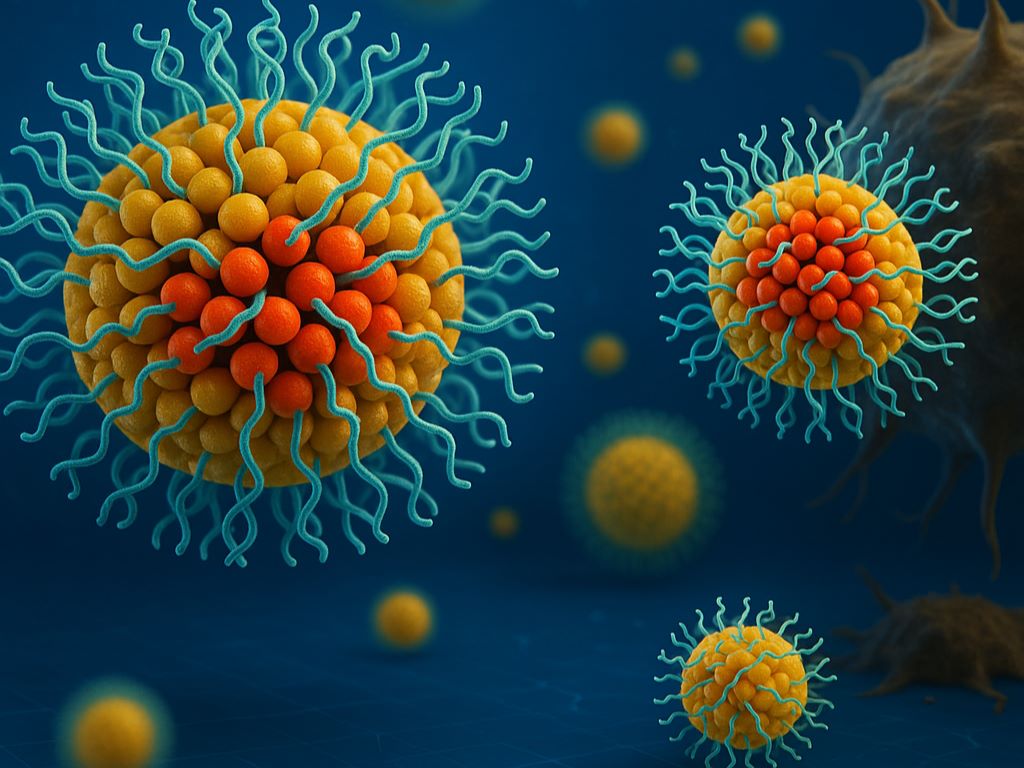
In the new study, the team designed a new drug from the ground up as a spherical nucleic acid (SNA): a nanostructure that weaves the drug directly into DNA strands coating tiny spheres. This design converts a poorly soluble, weakly performing drug into a powerful, targeted cancer killer that leaves healthy cells unharmed.
After developing the new therapy, the team tested it in a small animal model of acute myeloid leukaemia (AML), a fast-moving, difficult-to-treat blood cancer. Compared to the standard chemotherapy drug, the SNA-based drug entered leukaemia cells 12.5 times more efficiently, killed them up to 20 000 times more effectively and reduced cancer progression 59-fold – all without detectable side effects.
This work is another example of the potential of structural nanomedicine, a new field in which scientists use precise structural, as well as compositional, control to fine-tune how nanomedicines interact with the human body. With seven SNA-based therapies currently in clinical trials, the new approach could lead to potent vaccines and treatments for cancers, infectious diseases, neurodegenerative diseases and autoimmune diseases.
The study was published in the journal ACS Nano.
“In animal models, we demonstrated that we can stop tumors in their tracks,” said Northwestern’s Chad A. Mirkin, who led the study. “If this translates to human patients, it’s a really exciting advance. It would mean more effective chemotherapy, better response rates and fewer side effects. That’s always the goal with any sort of cancer treatment.”
For the new study, Mirkin and his team focused on the traditional chemotherapy drug 5-fluorouracil (5-Fu), which often fails to reach cancer cells efficiently. And, because it also attacks healthy tissue, 5-Fu causes myriad side effects, including nausea, fatigue and, in rare cases, even heart failure.
According to Mirkin, the drug itself is not the problem – it’s how the body processes it. 5-Fu is poorly soluble, meaning less than 1% of it dissolves in many biological fluids. Most drugs need to dissolve in the bloodstream before they can travel through the body to enter cells. If a drug is poorly soluble, it clumps or retains a solid form, and the body cannot absorb it efficiently.
“We all know that chemotherapy is often horribly toxic,” Mirkin said. “But a lot of people don’t realise it’s also often poorly soluble, so we have to find ways to transform it into water soluble forms and deliver it effectively.”
To develop a more effective delivery system, Mirkin and his team turned to SNAs. Invented and developed by Mirkin at Northwestern, SNAs are globular nanostructures with a nanoparticle core surrounded by a dense shell of DNA or RNA. In previous studies, Mirkin discovered that cells recognise SNAs and invite them inside. In the new study, his team built new SNAs with the chemotherapy chemically incorporated into the DNA strands.
“Most cells have scavenger receptors on their surfaces,” Mirkin said. “But myeloid cells overexpress these receptors, so there are even more of them. If they recognise a molecule, then they will pull it into the cell. Instead of having to force their way into cells, SNAs are naturally taken up by these receptors.”
As Mirkin and his team suspected, the structural redesign completely changed how 5-Fu interacted with the cancer cells. Unlike with free-floating, unstructured chemotherapy molecules, the myeloid cells easily recognised and absorbed the SNA form. Once inside, enzymes broke down the DNA shell to release the drug molecules, which killed the cancer cell from within.
In the mouse experiments, the therapy eliminated the leukaemia cells to near completion in the blood and spleen and significantly extended survival. And, because the SNAs selectively targeted AML cells, healthy tissues remained unharmed.
“Today’s chemotherapeutics kill everything they encounter,” Mirkin said. “So, they kill the cancer cells but also a lot of healthy cells. Our structural nanomedicine preferentially seeks out the myeloid cells. Instead of overwhelming the whole body with chemotherapy, it delivers a higher, more focused dose exactly where it’s needed.”
Next, Mirkin’s team plans to test the new strategy in a larger cohort of small animal models, then move to a larger animal model and, eventually, in human clinical trials, once funding is secured.
Source: Northwestern University





