Novel Therapy Saves Patient with Acute Fulminant Myocarditis
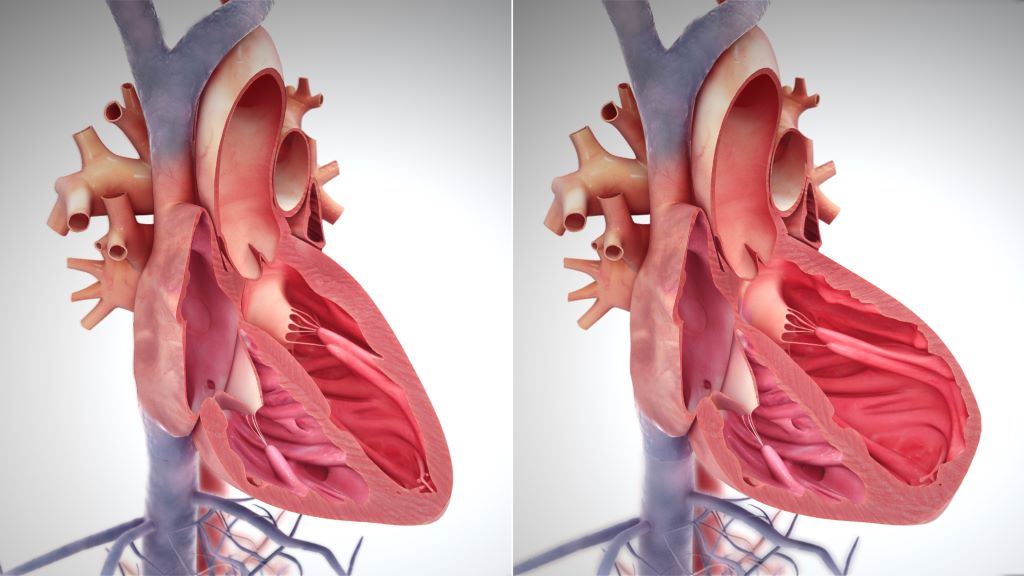
Acute myocarditis, or sudden inflammation of the heart, causes mild symptoms in most cases, but about 10% of acute myocarditis cases can be sudden and severe, leading to cardiac arrhythmias, heart pump failure, or even death. Current therapies for the condition are built on limited data and may not effectively target the underlying disease mechanisms. Patients may even require mechanical circulatory support for life support when the heart is failing.
Now a team at UC San Francisco is using a new class of drugs that target inflammation to treat acute fulminant myocarditis patients.
In an article in Circulation, the UCSF group reports on the successful treatment of a patient with sudden and severe (acute fulminant) myocarditis using an immune modulating medication known to inhibit the activity of enzymes that can trigger inflammation in the body.
“Our group has developed several animal models of myocarditis and by studying these, we became interested in a group of enzymes called Janus kinases, or JAKs, that seem to serve as communication nodes between immune cells,” said Javid Moslehi, MD, William Grossman Distinguished Professor in Cardiology and UCSF Section Chief of Cardio-Oncology and Immunology. “JAKs become hyperactive during acute heart inflammation, exacerbating the already activated immune system.”
Moslehi and his team therefore reasoned that targeting these enzymes using a novel class of therapies called JAK inhibitors would be a possible treatment modality for acute fulminant myocarditis. In recent years, the team has examined the effects of JAK inhibitor treatment on the immune cell populations for both RNA and proteins, showing acute benefit in various laboratory models of myocarditis.
Heart function improved dramatically
In the current case, the group treated a 20-year-old woman who came to UCSF with acute fulminant myocarditis.
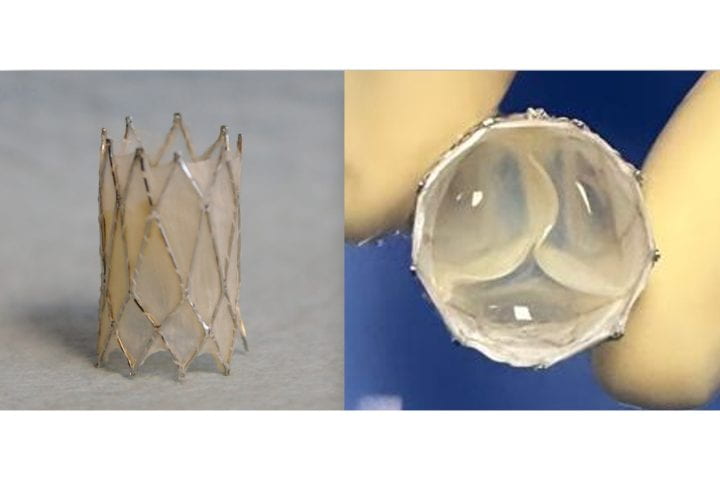
“This patient’s heart was effectively falling apart and there was no time to lose,” said Connor O’Brien, MD, cardiologist, critical care specialist and UCSF assistant professor of Medicine. “We had put the patient on extracorporeal membrane oxygenation (ECMO) to maintain blood flow through vital organs and started the process of listing her for heart transplantation.”
O’Brien was on clinical service at the time, caring for the patient. The medical team had tried using corticosteroids as a treatment but without success. O’Brien then coordinated with Moslehi, given his expertise in myocarditis as well as some of his laboratory results with JAK inhibitors.
O’Brien added ruxolitinib, a JAK inhibitor, to the treatment strategy. The patient’s cardiac arrhythmias slowed down and her cardiac enzyme (a measure of heart damage) decreased. Over the next few days, her heart function improved dramatically allowing her to wean off ECMO support. She was successfully discharged from the hospital one week later.
Since that time, the UCSF Health cardiology team has gone on to successfully treat other patients with JAK inhibitors for acute myocarditis, but Moslehi adds a note of caution.
“The gold standard of any new treatment is a clinical trial, and it is important to note that we have not yet done this,” said Moslehi. “But the team is hopeful that these early results can lead to an eventual trial for patients.”
Moslehi and his team established the UCSF Myocarditis Center in March 2023 as part of the newly formed section of cardio-oncology and immunology. This multi-disciplinary group is focused on diagnosis and treatment for myocarditis, bringing laboratory scientists together with clinicians for more comprehensive care of patients.
“The Myocarditis Center really takes advantage of the incredible scientific environment at UCSF and specifically our cardiology team working closely with the cardiovascular research institute (CVRI) to help our patients,” Moslehi adds.