Study Reveals Trained Immunity May Cause Lung Damage
Discovery could help explain why some people are more vulnerable to lung damage during severe inflammation

Trained immunity – a process being explored in vaccine and therapy development to boost immune defences – appears to be counterproductive in certain contexts, researchers at McGill University and the Research Institute of the McGill University Health Centre (The Institute) have found.
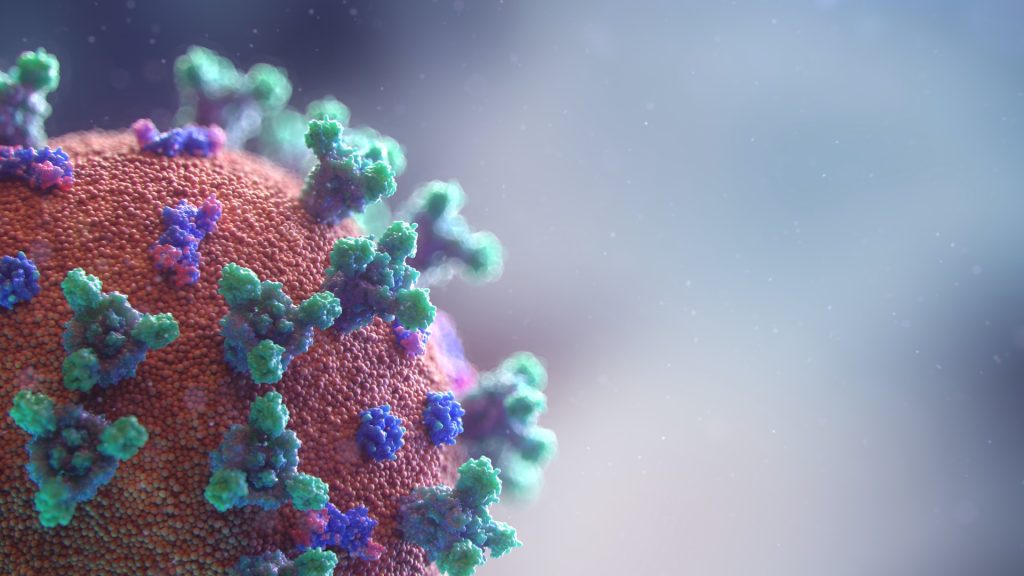
Trained immunity is when the body’s first line of defence remembers past threats and becomes more reactive, responding more strongly to future infections even if they are different, by changing immune cells’ behaviour.
In an earlier study, the researchers had determined beta-glucan, a molecule found in the cell walls of fungi like yeast and mushrooms, can reduce lung damage during influenza infection. That study had focused on beta-glucan’s impact on neutrophils.
However, in a new study, published in the journal eLife, the team found exposure to beta-glucan can reprogram alveolar macrophages in a way that worsens lung damage during severe inflammation caused by viral or bacterial products. These cells help keep the lungs clean by clearing out dust, debris and pathogens.
“To date, most trained immunity research has focused on circulating immune cells that arise from the bone marrow,” said lead author Renaud Prével, a postdoctoral fellow at the Meakins-Christie Laboratories at The Institute. “We wanted to explore whether beta-glucan could induce trained immunity in alveolar macrophages, and whether that might be helpful or harmful.”
The researchers exposed mice to beta-glucan, which is known to trigger trained immunity and is found in some health supplements. A week later, the mice were exposed to signals that mimic severe viral or bacterial infections with sepsis-like phenotype. Using high-resolution microCT scans and fluid analysis, they found that mice given beta-glucan developed significantly more severe lung damage compared to the untreated control group.
To confirm the immune cells were causing the damage, researchers removed them from the mice, and the inflammation went away. When they put trained alveolar macrophages into other mice, the inflammation came back. The cells showed signs of immune training, but surprisingly, this didn’t happen through the usual immune pathways. It needed signals from infections and help from other immune cells.
“Our study shows that immune memory in the lungs is more dynamic than previously thought,” said senior author Maziar Divangahi, Professor of Medicine at McGill and Associate Director of the Meakins-Christie Laboratories. “This could help explain why some individuals develop more severe lung inflammation, especially in settings like sepsis.”
Source: McGill University